Chapter 10 Motor System
10.1 Spinal Motor Control and Proprioception
The motor system refers to the nerve cells that are used to control our body. The key roles of the motor system are to plan, control, and execute voluntary (deliberate) movements, and to control involuntary (subconscious or automatic) functions, such as digesting food. The motor system is sometimes described as a top-down process: in a voluntary movement, neural activity in the frontal lobe sends commands down to motor neurons located in the brainstem or spinal cord, which in turn activate muscle groups. In reality, motor control is more of a loop, rapidly communicating between the sensory cortex and motor cortex. Sensory information about limb position, posture, and objects in contact with the skin inform the descending motor plan. Simultaneously, the motor plan provides predictions about upcoming movement.
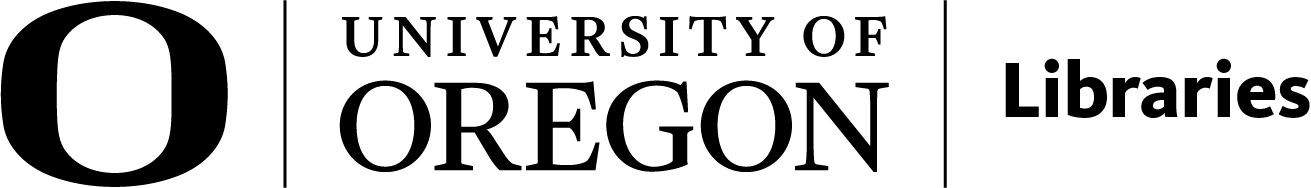
There are multiple levels of control. Within the spinal cord, simple reflexes can function without higher input from the brain. Slightly more complex spinal control occurs when central pattern generators function during repetitive movements like walking. The motor and premotor cortices in the brain are responsible for the planning and execution of voluntary movements. And finally, the basal ganglia and cerebellum modulate the responses of the neurons in the motor cortex to help with coordination, motor learning, and balance.
This lesson explores the lowest level of control at the level of the spinal cord.
Alpha Motor Neurons
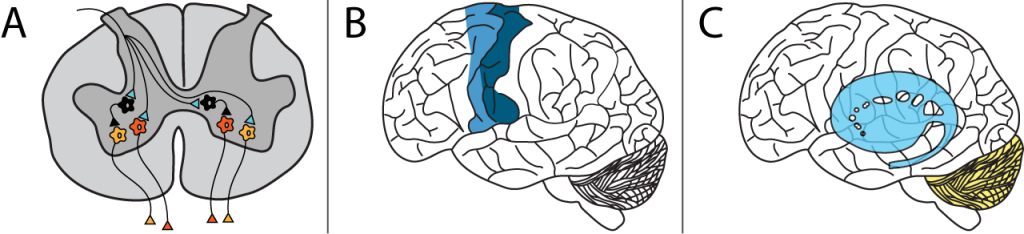
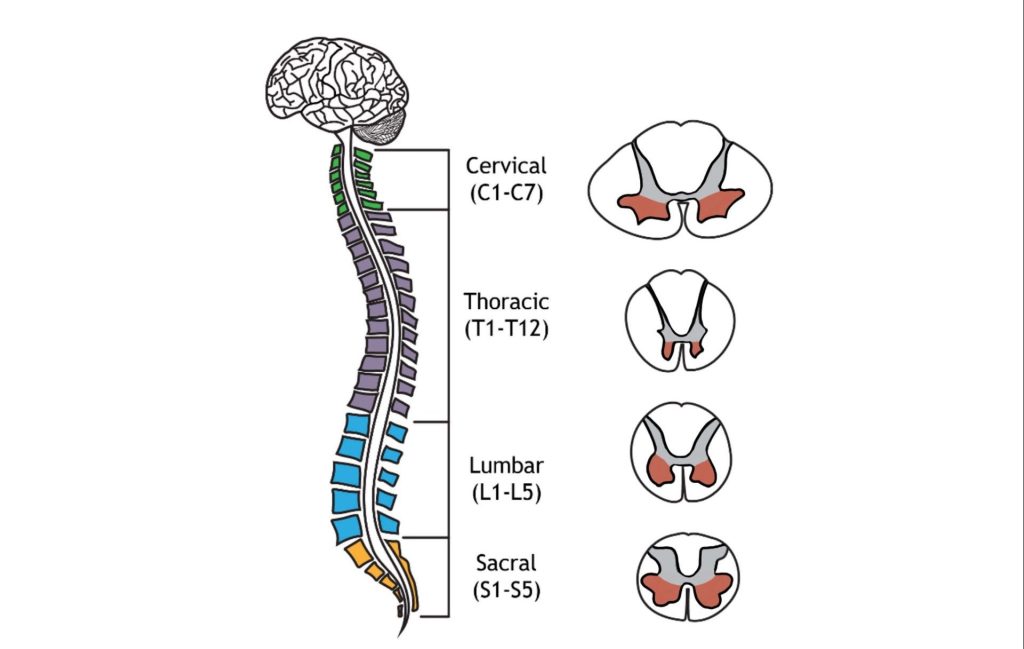
Muscle fibers are innervated by alpha motor neurons. Alpha motor neurons are also called lower motor neurons because they are not located in higher brain areas. These cells are the only cells that directly command muscle contraction. The cell bodies of the alpha motor neurons are located in the central nervous system in the ventral horn of the spinal cord. Their axons leave the spinal cord via the ventral roots and travel to the muscle via efferent peripheral spinal nerves.
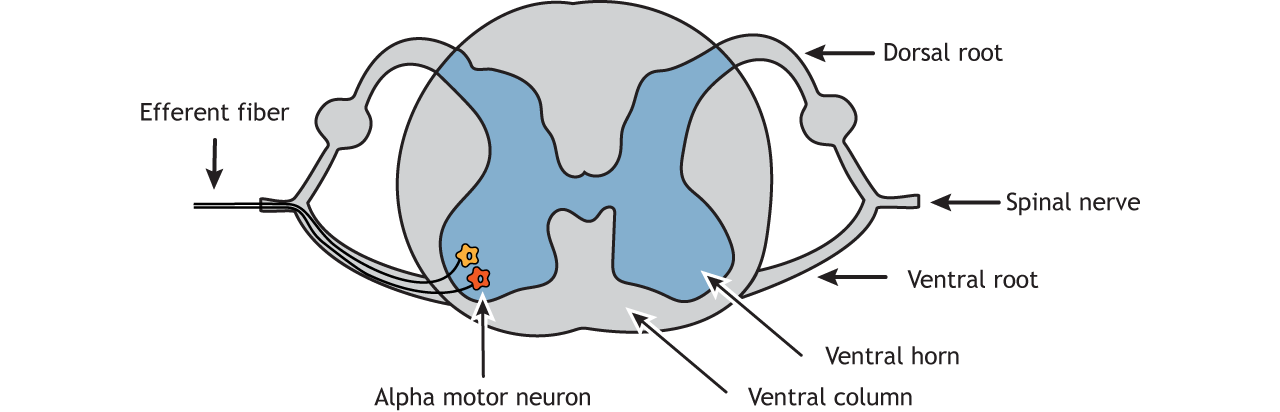
Like the sensory systems, the motor system is also organized in a topographic fashion, referred to as ‘somatotopic organization’. Within the spinal cord, alpha motor neurons that innervate muscles in the arms and legs are located in the lateral portion of the ventral horn, whereas alpha motor neurons that innervate muscles in the trunk are located in the medial portion.
Location of Alpha Motor Neurons
The structure of the spinal cord is reviewed in Chapter 26 of Introduction to Neurobiology. Examining cross sections of the spinal cord at different levels reveals that there is a non-uniform distribution of lower motor neurons. This is determined by the size of the ventral horn at the different levels of the spinal cord. At the cervical enlargement the larger ventral horns are due to the presence of more lower motor neurons that function in movement of the arms. At the lumbar enlargement the larger ventral horns are due to the presence of more lower motor neurons that function in movement of the legs.
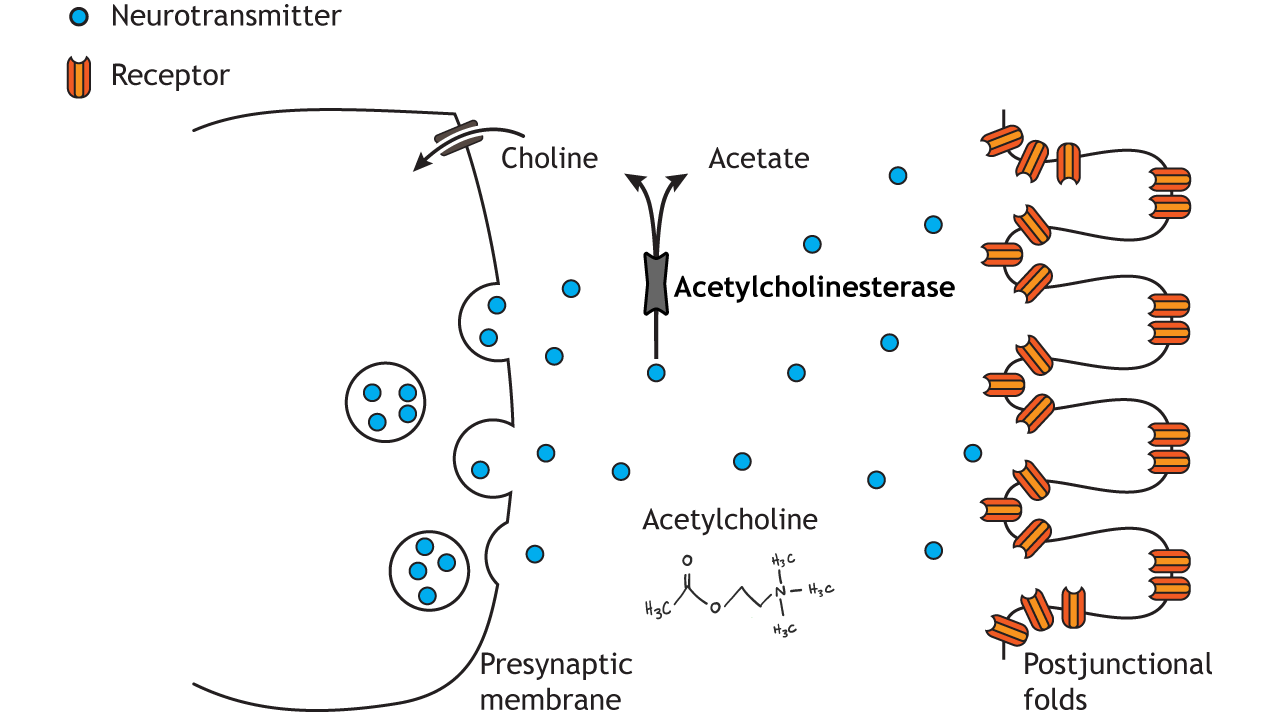
Neuromuscular Junction
The lower motor neurons communicate with muscle fibers (muscle cells) at the neuromuscular junction (NMJ). The NMJ is similar to other chemical synapses, however the postsynaptic cell is a muscle cell separated by about 30 nm. The presynaptic cell is the motor neuron and the postsynaptic site is the sarcolemma, the cell membrane of the long cylindrical muscle fibers (muscle cells). The neuromuscular junction is one of the largest synapses in the body and one of the most well-studied because of its peripheral location.
The neuromuscular junction is located midway down the length of the muscle fiber. The muscle fiber will contract in response to depolarization traveling down the sarcolemma of the muscle fiber. The synapse is located midway down the length of the muscle fiber so that the postsynaptic signal can travel in both directions down the long muscle fiber and quickly activate a contraction along the entire cell.
Acetylcholine is the neurotransmitter released at the neuromuscular junction (NMJ), and it acts upon ligand-gated, non-selective cation channels called nicotinic acetylcholine receptors that are present in postjunctional folds of the muscle fiber. Nicotinic acetylcholine receptors allow the influx of sodium ions into the muscle cell. The depolarization will cause nearby voltage-gated channels to open and fire an action potential in the muscle fiber. In a healthy system, an action potential in the motor neurons always causes an action potential in the muscle cell. The action potential leads to contraction of the muscle fiber.
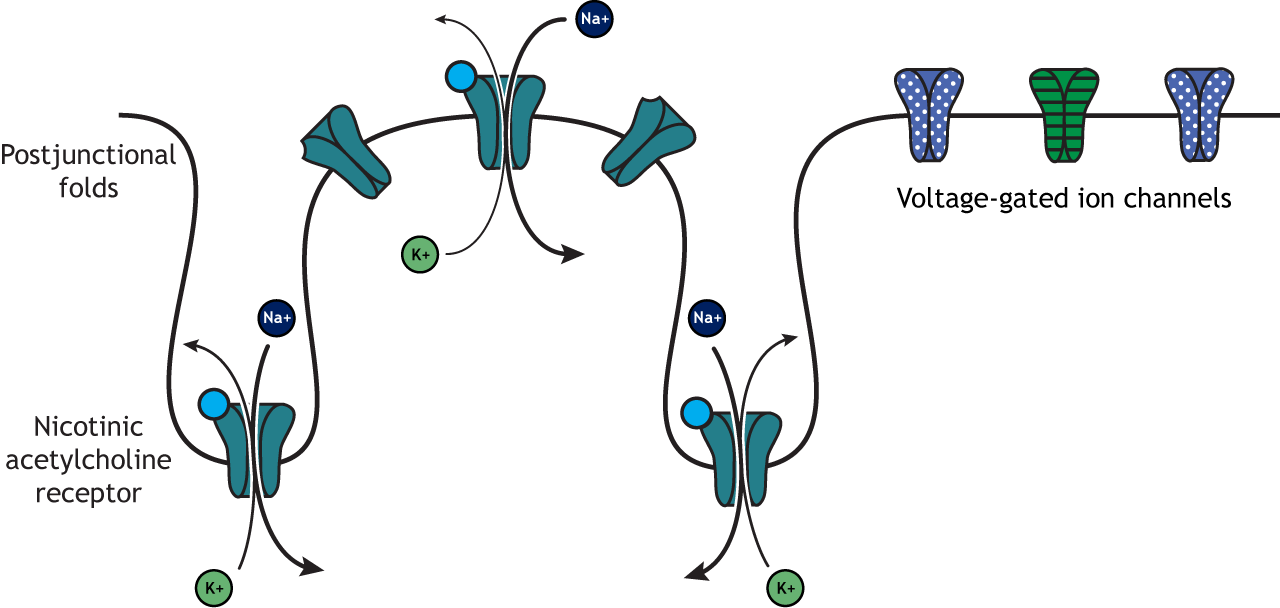
To review, an action potential traveling down the motor neuron (presynaptic cell) will cause the release of acetylcholine into the synapse. Acetylcholine binds to postsynaptic nicotinic acetylcholine receptors that are located in the folded sarcolemma (increasing surface area), causing depolarization of muscle fibers and ultimately muscle contraction.
Acetylcholinesterase, an enzyme that breaks down acetylcholine and terminates its action, is present in the synaptic cleft of the neuromuscular junction. Muscle contraction must be tightly controlled. Thus, the actions of acetylcholinesterase are very important to cease muscle contraction quickly.
Clinical Application: Myasthenia gravis
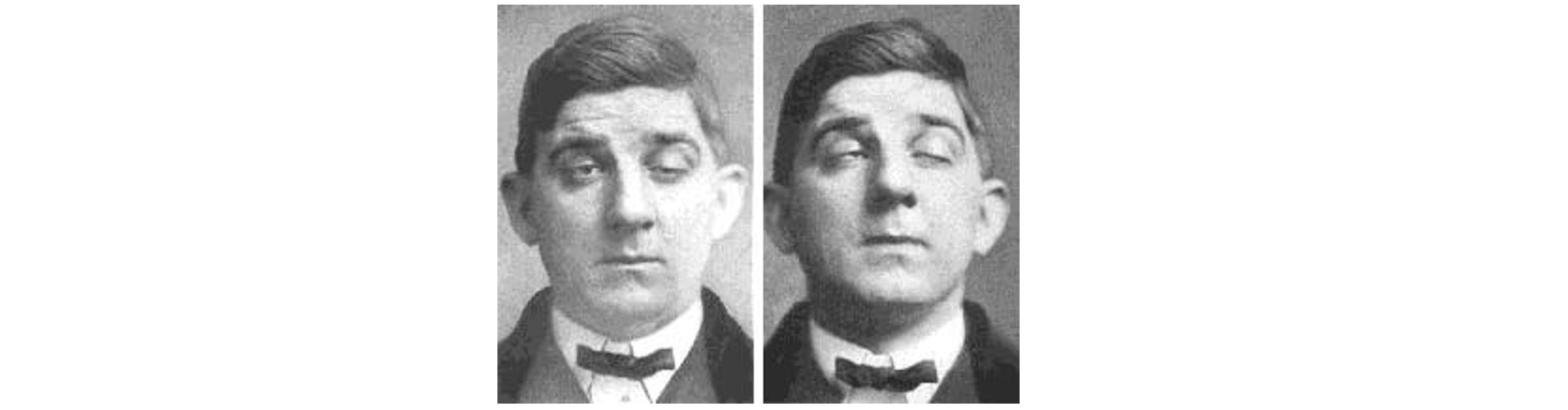
Myasthenia gravis (MG) is an autoimmune disorder characterized by muscle weakness, resulting in difficulty with speech, trouble with movement and swallowing, drooping eyelids, and double vision. Each year, an estimated 20 out of a million people get diagnosed with MG.
The muscle weakness seen in MG results from immune system-mediated destruction of the nicotinic acetylcholine receptors expressed at the NMJ. Thus, when the lower motor neuron releases acetylcholine, the muscle cells are unable to detect this release, so they fail to contract appropriately.
One therapeutic strategy involves inhibition of acetylcholinesterase, the enzyme that degrades acetylcholine. This causes the synaptic acetylcholine to remain in the synapse longer, increasing the chance that receptors get activated. Alternatively, autoimmune diseases like MG can be improved with immunosuppressant therapy. With successful treatment, MG usually does not result in changes in lifespan.
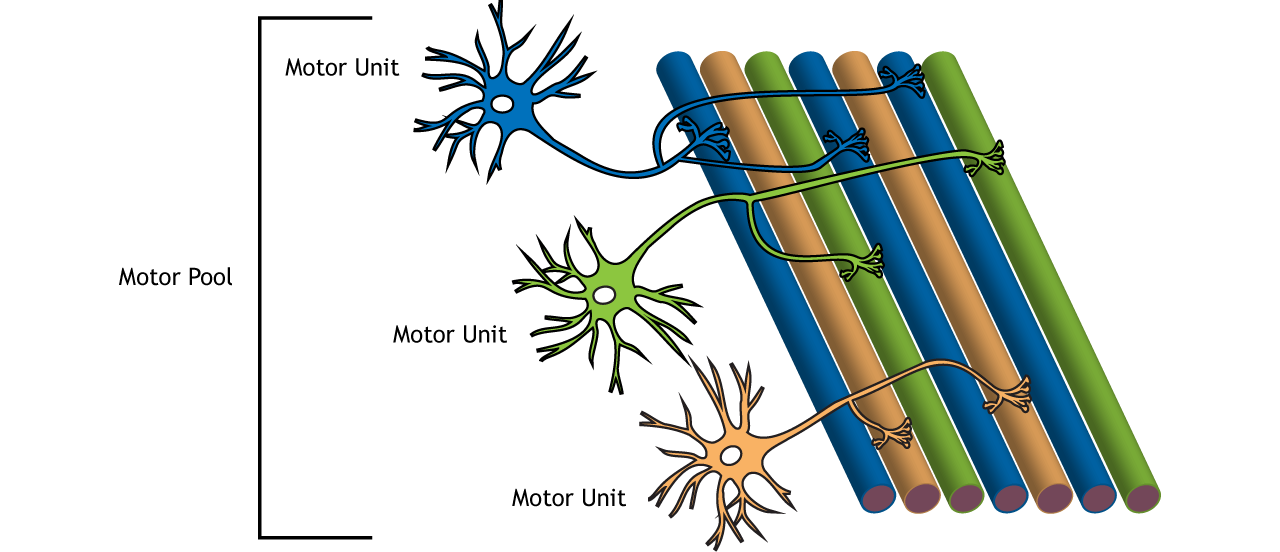
Motor Units
Importantly, there are many more muscles cells than there are motor neurons. One alpha motor neuron can innervate multiple fibers within one muscle due to the branching of motor neuron axons. Each axon terminal synapses (innervates) a single muscle fiber. A motor neuron and all the fibers innervated by it are called a motor unit. The muscle fibers within one motor unit are often spread throughout the muscle to spread the contraction throughout the full muscle. Further, motor units in a muscle usually contract asynchronously to help protect the muscle from fatigue. A graded contraction of the muscle is produced by activating varying numbers of motor units.
Motor units differ in size. Small motor units are motor units that innervate fewer muscle fibers and thus control fine movements. Small motor units are located in the eyes and fingers, both of which function in fine and precise movements. Large motor units innervate many muscle fibers and are typically found in weight-bearing muscles like the thighs.
The group of motor neurons that innervate all the fibers of one muscle is called a motor pool.
Types of Motor Units
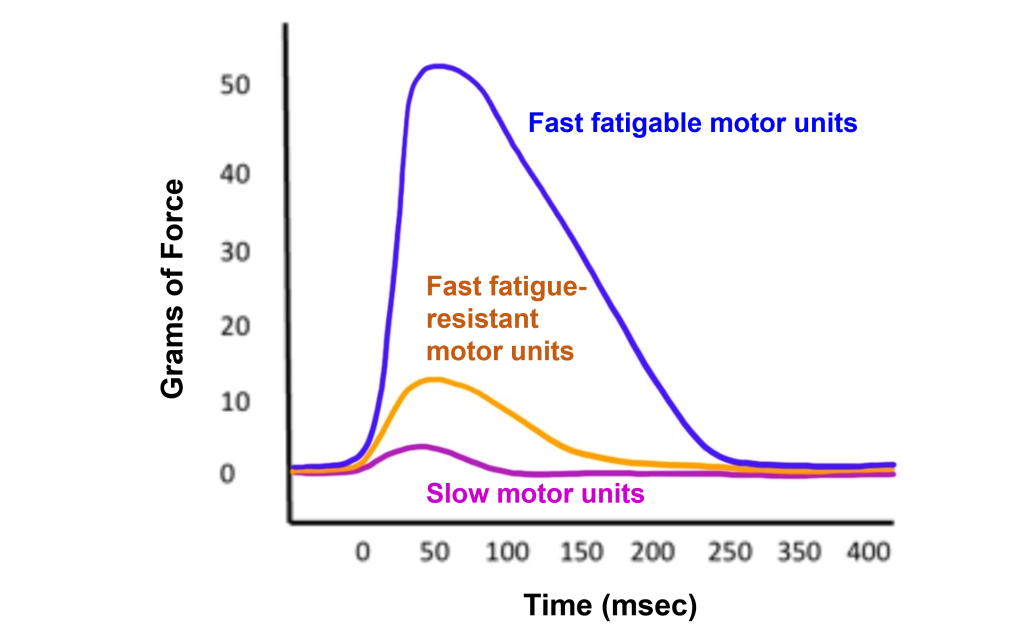
In addition to the size of the motor unit, the types of muscle fibers that are innervated by motor units can also differ. There are three different types of motor units:
- Slow motor units. Slow motor units are slow to contract and generate less force but can work for a long time. They are used in endurance exercise like jogging.
- Fast fatigue-resistant motor units. Fast fatigue-resistant motor units are quick to contract (though not as fast the fast fatigable motor units). These motor units generate more force that then slow motor units, but are much more resistant to fatigue than the fast fatigable motor units.
- Fast fatigable motor units. Fast fatigable motor units are quickest to contract and generate the most force. These motor units are more prone to fatigue due to decreased number of mitochondria within the muscles. Fast fatigable motor units generate a lot of force quickly, but also tire quickly. They are used mostly in high intensity exercise like lifting weights and sprinting.
Muscle Activation
Action Potential Triggered in a Muscle
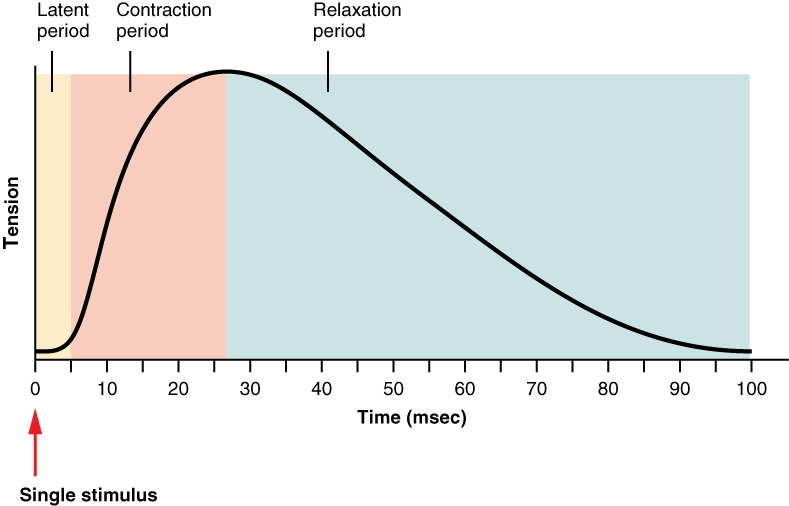
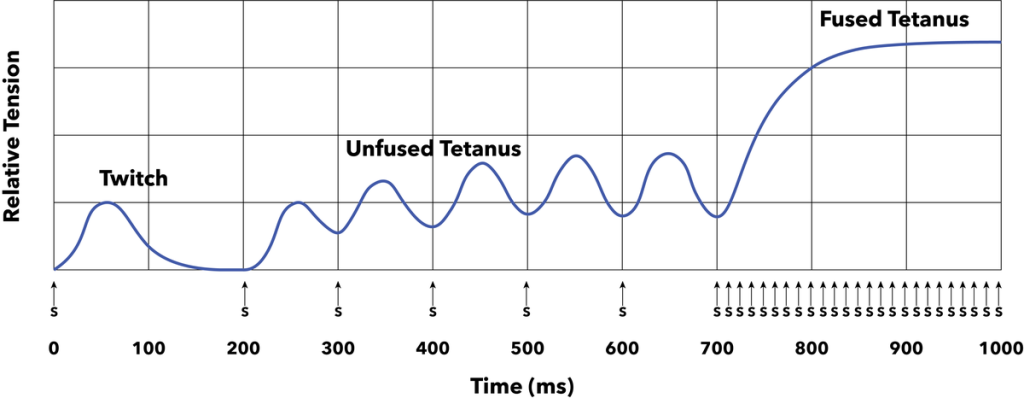
When an action potential is triggered in a muscle it causes a muscle twitch (contraction) that is followed by a period of relaxation. A muscle twitch shows an increase in tension after a short delay (latent period). During the contraction period, the muscle tension increased, and then has a long relaxation period, causing the muscle tension to be increased long after the initial stimulus.
When a stimulus occurs during the long relaxation period following a muscle twitch, the newly generated muscle twitch will summate to increase the strength of the overall muscle contraction. Shortening the time between stimuli will result in unfused tetanus and if stimuli are very close together will result in fused tetanus. Therefore, a higher rate of action potentials in the alpha motor neuron will generate more muscle contraction.
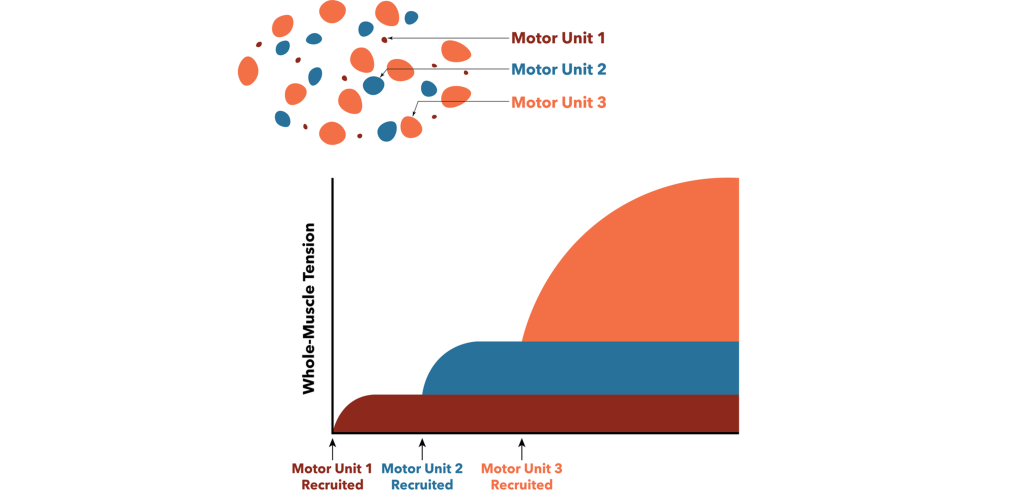
Muscle Recruitment
In addition to the rate of action potentials changing the force of the muscle contraction, muscle recruitment can also increase the strength of contraction within a muscle. When generating motor activity, the smallest motor units will be activated to contract first due to their size and increased excitability to move the load. Increasingly larger motor units are recruited to lift heavier loads. Recruitment of motor units allows for us to generate appropriate muscle tension to move a given load. For example, if you need to pick up a pencil, then we do not need to use the same force as if we were trying to pick up a 20-pound weight. Only smaller motor units would be activated to pick up the pencil, and increasingly larger motor units would be recruited to lift the heavier load of the 20-pound weight.
Alpha Motor Neuron Inputs
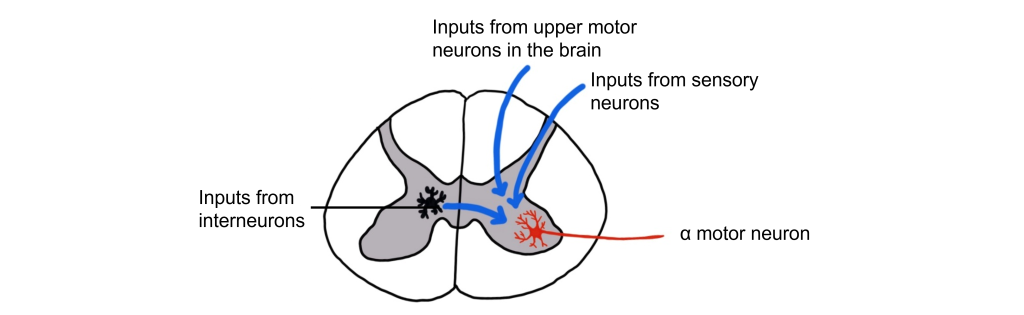
The alpha motor neurons that directly cause muscle contraction receive inputs from three different sources.
- Sensory cells from the dorsal root ganglion that provide sensory information from the muscles through proprioception.
- Upper motor neurons from the motor cortex in the brain and brain stem that are responsible for initiating voluntary movement.
- Interneurons in the spinal cord. These represent the largest input to the alpha motor neurons and can either provide excitation or inhibition to the alpha motor neuron.
Proprioception
Raise your arms above your head. Even without seeing your arms, your nervous system has mechanisms that inform you about the location and position of your body parts, including how much your joints are bent. This sense is called proprioception and is critically important for coordinated movement and motor reflexes that contribute to those tiny, rapid adjustments that are made while maintaining balance. Proprioceptive information ascends through the spinal cord and into the brain via the dorsal column-medial lemniscus tract. Proprioception is also processed in the primary somatosensory cortex.
Proprioception refers to the “body sense” that informs us about how our bodies are positioned and moving in space. Proprioceptors are receptors that provide proprioception information.
There are two main types of proprioceptors:
- Muscle spindles measure muscle stretch (muscle length) and transmit this sensory information via 1a sensory afferent fibers. Muscle spindles are nested within and arranged parallel to the extrafusal muscle fibers.
- Golgi Tendon Organs measure muscle tension and transmit this sensory information via 1b sensory afferent fibers. Golgi tendon organs are located between the extrafusal muscle fibers and their points of attachment at the bone.
Muscle Spindles
Extrafusal and Intrafusal Muscle Fibers
Muscle spindles are fibrous capsules that are located within muscles. Intrafusal muscle fibers are special muscle fibers that are located within the fibrous capsule of the muscle spindle. The intrafusal muscle fibers are innervated by gamma motor neurons that will cause them to contract.
Extrafusal muscle fibers, however, make up the bulk of the muscle and are located outside of the muscle spindle. The extrafusal muscle fibers are stimulated to contract by the alpha motor neurons.
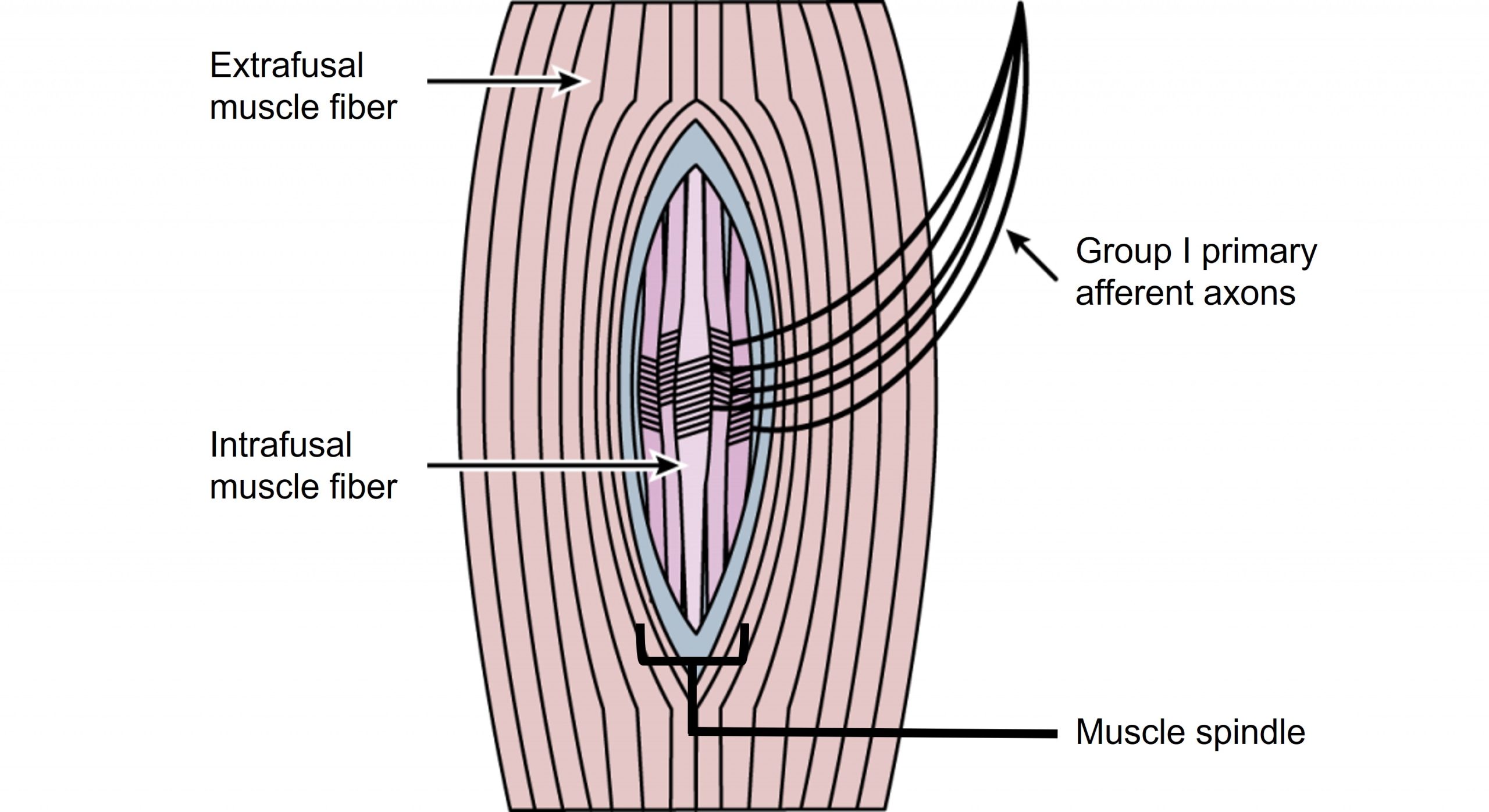
Muscle Spindles Function
Group 1a sensory afferent axons, which have a large diameter and are heavily myelinated, wrap around the intrafusal fibers contained within the muscle spindle. These sensory afferent fibers will signal when the intrafusal fibers of the muscle spindle are experiencing stretch and communicate information about muscle length.
Within the spinal cord, a single sensory 1a afferent axon synapses on every alpha motor neuron within the motor pool that innervates the muscle that contains the muscle spindle. This allows for a fast and powerful contraction of the muscle in response to a change in muscle stretch.
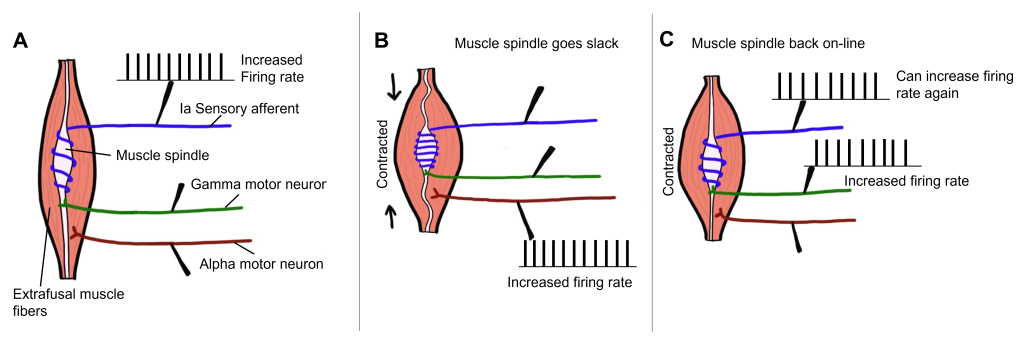
Gamma Motor Neuron Function
When the muscle experiences a stretch and the extrafusal fibers are stretched, the muscle spindle and the intrafusal fibers are also stretched (due to being within the muscle and surrounded by the extrafusal fibers). When the muscle spindle stretches, the 1a sensory axon will start to fire action potentials. The sensory axon synapses with an alpha motor neuron that will then cause the extrafusal muscle fibers to contract. As the extrafusal fibers contract and the muscle shortens, the muscle spindle goes slack, and the 1a axon will no longer fire action potentials as it is no longer being stretched. The gamma motor neuron is then activated that innervates the intrafusal muscle fibers, causing the intrafusal fibers to contract, allowing the muscle spindle to sense stretch again. Therefore, the gamma motor neuron is critical for allowing the muscle spindle to continue providing information about muscle stretch even when the muscle has experienced contraction.
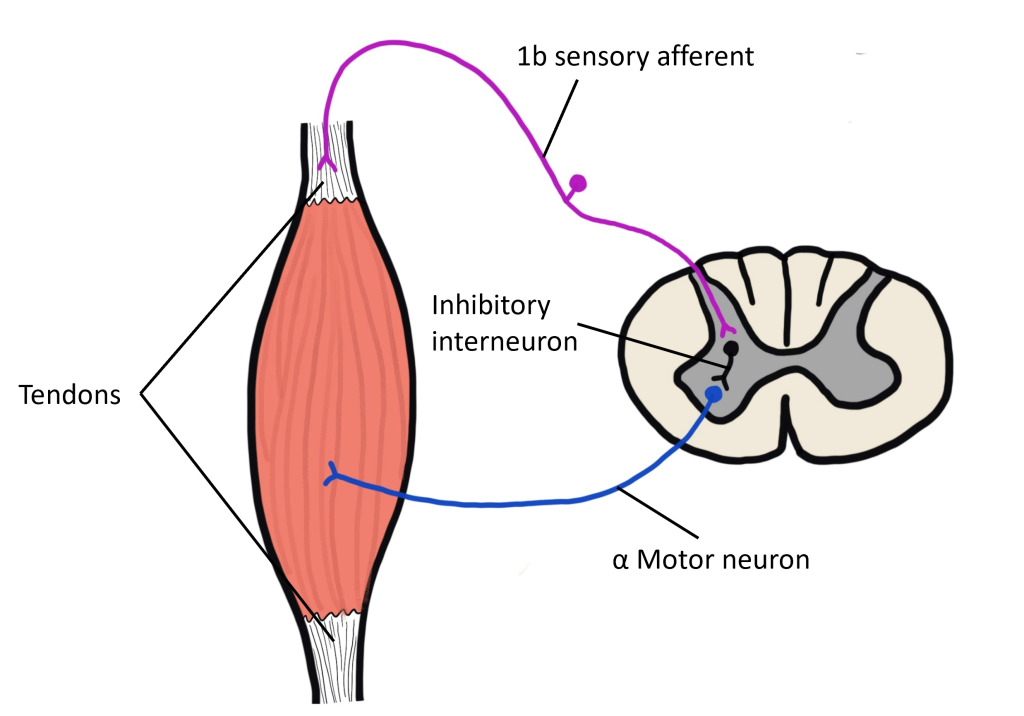
Golgi Tendon Organ
The Golgi tendon organ is a proprioceptor that measures muscle tension, or the force of contraction. They also contribute to our detection of weight, as we lift something heavy for example. Golgi tendon organs are located in the tendon that connects the muscle to bone. The tendon is made up of collagen fibrils and the Group 1b sensory axons are intertwined within the collagen fibrils. When the muscle experiences an increase in tension, the collagen fibrils surrounding the 1b sensory axon physically squeeze the 1b axon, opening mechanically-gated ion channels within the 1b sensory axon.
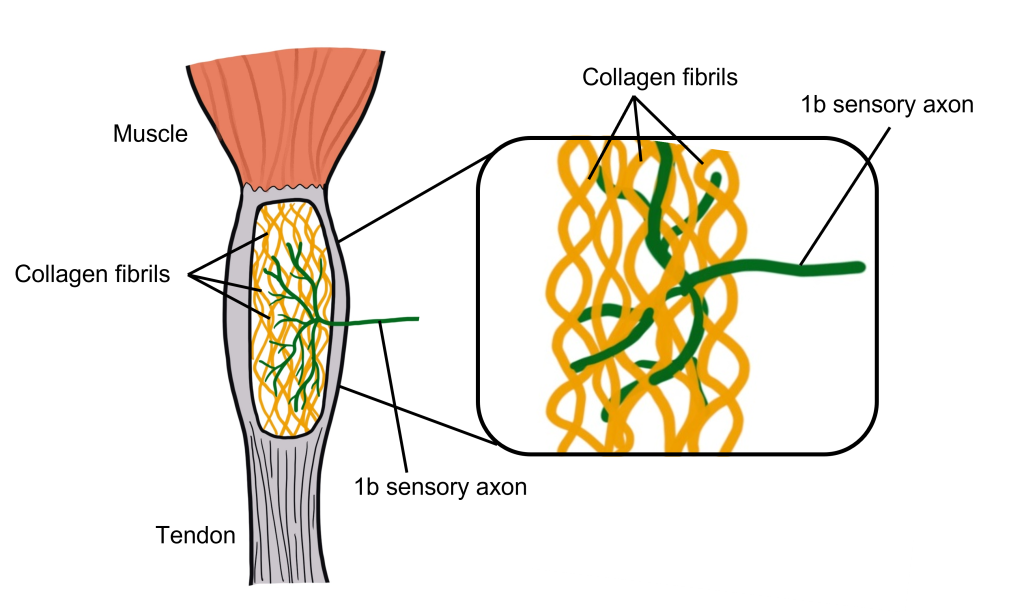
The purpose of the Golgi tendon organ is to allow for an optimal range of tension for the muscle and to protect the muscle from injury due to being overloaded. This is accomplished through a negative feedback loop controlled by the Golgi tendon organ. When the muscle experiences an increase in muscle tension, the 1b sensory axon starts to fire action potentials. The sensory neuron synapses onto an inhibitory interneuron within the spinal cord, which when active will release GABA onto the alpha motor neuron that innervates the same muscle that experienced the increase in muscle tension to begin with. When GABA binds to the alpha motor neuron, it will decrease firing of the alpha motor neuron, leading to a decrease in contraction of the muscle. This is an example of negative feedback as the increased muscle tension ultimately leads to physiological changes that decrease muscle tension.
Key Takeaways
- Motor neuron cell bodies are located in the ventral horn of the spinal cord.
- Motor neuron axons are located in the peripheral nervous system and travel to muscles via spinal nerves.
- Acetylcholine is released at the neuromuscular junction and acts upon ionotropic nicotinic acetylcholine receptors.
- The spinal cord is topographically organized.
- Muscle twitches can summate to increase muscle tension.
- A motor unit is an alpha motor neuron and all of the motor fibers that it innervates. Motor units differ in size, recruitment, and power.
- Muscle spindles and Golgi tendon organs are proprioceptors that communicate information about the location and position of the body.
Test Yourself!
Additional Review
- What is the difference between a motor unit and a motor pool?
Attributions
This chapter is adapted from 32. Spinal Motor Control and Proprioception in Introduction to Neurobiology by Avinash Singh which is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License. Which is adapted from “Spinal Motor Control and Proprioception” in Introduction to Neuroscience by Valerie Hedges which is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Media Attributions
- MotorControlRegions © Casey Henley adapted by Valerie Hedges is licensed under a CC BY-NC-SA (Attribution NonCommercial ShareAlike) license
- Alpha Motor Neuron © Casey Henley adapted by Valerie Hedges is licensed under a CC BY-NC-SA (Attribution NonCommercial ShareAlike) license
- Spinal Cord Map © Casey Henley adapted by Valerie Hedges is licensed under a CC BY-NC-SA (Attribution NonCommercial ShareAlike) license
- Untitled_Artwork 1 © Casey Henley adapted by Valerie Hedges is licensed under a CC BY-NC-SA (Attribution NonCommercial ShareAlike) license
- NMJ Ion Flow © Casey Henley adapted by Valerie Hedges is licensed under a CC BY-NC-SA (Attribution NonCommercial ShareAlike) license
- NeuromuscularJunction © Casey Henley adapted by Valerie Hedges is licensed under a CC BY-NC-SA (Attribution NonCommercial ShareAlike) license
- Myasthenia Gravis © Posey and Spiller adapted by Valerie Hedges is licensed under a Public Domain license
- Motor Unit And Pool © Casey Henley adapted by Valerie Hedges is licensed under a CC BY-NC-SA (Attribution NonCommercial ShareAlike) license
- Types of motor units © Valerie Hedges is licensed under a CC BY-NC-SA (Attribution NonCommercial ShareAlike) license
- Muscle_Twitch_Myogram © OpenStax adapted by Valerie Hedges is licensed under a CC BY (Attribution) license
- Twitch_vs_unfused_tetanus_vs_fused_tetanus © Daniel Walsh and Alan Sved adapted by Valerie Hedges is licensed under a CC BY-SA (Attribution ShareAlike) license
- Motor unit recruitment © Daniel Walsh and Alan Sved is licensed under a CC BY-SA (Attribution ShareAlike) license
- Motor neuron inputs © Valerie Hedges is licensed under a CC BY-NC-SA (Attribution NonCommercial ShareAlike) license
- Muscle Spindle © Casey Henley adapted by Valerie Hedges is licensed under a CC BY-NC-SA (Attribution NonCommercial ShareAlike) license
- Gamma motor neuron function © Valerie Hedges is licensed under a CC BY-NC-SA (Attribution NonCommercial ShareAlike) license
- Golgi tendon organ © Valerie Hedges is licensed under a CC BY-NC-SA (Attribution NonCommercial ShareAlike) license
- golgi tendon organ signaling © Valerie Hedges is licensed under a CC BY-NC-SA (Attribution NonCommercial ShareAlike) license
Learning Objectives
By the end of this section, you will be able to:
- Explain how hormonal cues help the kidneys synchronize the osmotic needs of the body
- Describe how hormones like epinephrine, norepinephrine, renin-angiotensin, aldosterone, anti-diuretic hormone, and atrial natriuretic peptide help regulate waste elimination, maintain correct osmolarity, and perform other osmoregulatory functions
While the kidneys operate to maintain osmotic balance and blood pressure in the body, they also act in concert with hormones. Hormones are small molecules that act as messengers within the body. Hormones are typically secreted from one cell and travel in the bloodstream to affect a target cell in another portion of the body. Different regions of the nephron bear specialized cells that have receptors to respond to chemical messengers and hormones. Table 4.1 summarizes the hormones that control the osmoregulatory functions.
| Hormone | Where produced | Function |
|---|---|---|
| Epinephrine and Norepinephrine | Adrenal medulla | Can decrease kidney function temporarily by vasoconstriction |
| Renin | Kidney nephrons | Increases blood pressure by acting on angiotensinogen |
| Angiotensin | Liver | Angiotensin II affects multiple processes and increases blood pressure |
| Aldosterone | Adrenal cortex | Prevents loss of sodium and water |
| Anti-diuretic hormone (vasopressin) | Hypothalamus (stored in the posterior pituitary) | Prevents water loss |
| Atrial natriuretic peptide | Heart atrium | Decreases blood pressure by acting as a vasodilator and increasing glomerular filtration rate; decreases sodium reabsorption in kidneys |
Epinephrine and Norepinephrine
Epinephrine and norepinephrine are released by the adrenal medulla and nervous system respectively. They are the flight/fight hormones that are released when the body is under extreme stress. During stress, much of the body’s energy is used to combat imminent danger. Kidney function is halted temporarily by epinephrine and norepinephrine. These hormones function by acting directly on the smooth muscles of blood vessels to constrict them. Once the afferent arterioles are constricted, blood flow into the nephrons stops. These hormones go one step further and trigger the renin-angiotensin-aldosterone system.
Renin-Angiotensin-Aldosterone
The renin-angiotensin-aldosterone system, illustrated in Figure 4.15 proceeds through several steps to produce angiotensin II, which acts to stabilize blood pressure and volume. Renin (secreted by a part of the juxtaglomerular complex) is produced by the granular cells of the afferent and efferent arterioles. Thus, the kidneys control blood pressure and volume directly. Renin acts on angiotensinogen, which is made in the liver and converts it to angiotensin I. Angiotensin converting enzyme (ACE) converts angiotensin I to angiotensin II. Angiotensin II raises blood pressure by constricting blood vessels. It also triggers the release of the mineralocorticoid aldosterone from the adrenal cortex, which in turn stimulates the renal tubules to reabsorb more sodium. Angiotensin II also triggers the release of anti-diuretic hormone (ADH) from the hypothalamus, leading to water retention in the kidneys. It acts directly on the nephrons and decreases glomerular filtration rate. Medically, blood pressure can be controlled by drugs that inhibit ACE (called ACE inhibitors).
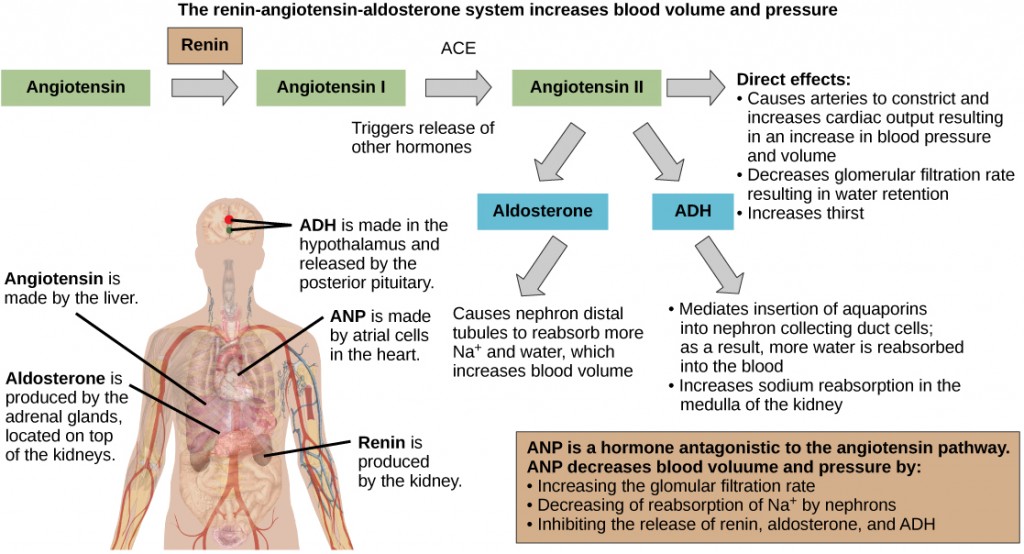
Mineralocorticoids
Mineralocorticoids are hormones synthesized by the adrenal cortex that affect osmotic balance. Aldosterone is a mineralocorticoid that regulates sodium levels in the blood. Almost all of the sodium in the blood is reclaimed by the renal tubules under the influence of aldosterone. Because sodium is always reabsorbed by active transport and water follows sodium to maintain osmotic balance, aldosterone manages not only sodium levels but also the water levels in body fluids. In contrast, the aldosterone also stimulates potassium secretion concurrently with sodium reabsorption. In contrast, absence of aldosterone means that no sodium gets reabsorbed in the renal tubules and all of it gets excreted in the urine. In addition, the daily dietary potassium load is not secreted and the retention of K+ can cause a dangerous increase in plasma K+ concentration. Patients who have Addison's disease have a failing adrenal cortex and cannot produce aldosterone. They lose sodium in their urine constantly, and if the supply is not replenished, the consequences can be fatal.
Antidiurectic Hormone
As previously discussed, antidiuretic hormone or ADH (also called vasopressin), as the name suggests, helps the body conserve water when body fluid volume, especially that of blood, is low. It is formed by the hypothalamus and is stored and released from the posterior pituitary. It acts by inserting aquaporins in the collecting ducts and promotes reabsorption of water. ADH also acts as a vasoconstrictor and increases blood pressure during hemorrhaging.
Atrial Natriuretic Peptide Hormone
The atrial natriuretic peptide (ANP) lowers blood pressure by acting as a vasodilator. It is released by cells in the atrium of the heart in response to high blood pressure and in patients with sleep apnea. ANP affects salt release, and because water passively follows salt to maintain osmotic balance, it also has a diuretic effect. ANP also prevents sodium reabsorption by the renal tubules, decreasing water reabsorption (thus acting as a diuretic) and lowering blood pressure. Its actions suppress the actions of aldosterone, ADH, and renin.
Summary
Hormonal cues help the kidneys synchronize the osmotic needs of the body. Hormones like epinephrine, norepinephrine, renin-angiotensin, aldosterone, anti-diuretic hormone, and atrial natriuretic peptide help regulate the needs of the body as well as the communication between the different organ systems.
Exercises
- Renin is made by ________.
- granular cells of the juxtaglomerular apparatus
- the kidneys
- the nephrons
- All of the above.
- Patients with Addison's disease ________.
- retain water
- retain salts
- lose salts and water
- have too much aldosterone
- Which hormone elicits the “fight or flight” response?
- epinephrine
- mineralcorticoids
- anti-diuretic hormone
- thyroxine
- Describe how hormones regulate blood pressure, blood volume, and kidney function.
- How does the renin-angiotensin-aldosterone mechanism function? Why is it controlled by the kidneys?
Answers
- a
- c
- a
- Hormones are small molecules that act as messengers within the body. Different regions of the nephron bear specialized cells, which have receptors to respond to chemical messengers and hormones. The hormones carry messages to the kidney. These hormonal cues help the kidneys synchronize the osmotic needs of the body. Hormones like epinephrine, norepinephrine, renin-angiotensin, aldosterone, anti-diuretic hormone, and atrial natriuretic peptide help regulate the needs of the body as well as the communication between the different organ systems.
- The renin-angiotensin-aldosterone system acts through several steps to produce angiotensin II, which acts to stabilize blood pressure and volume. Thus, the kidneys control blood pressure and volume directly. Renin acts on angiotensinogen, which is made in the liver and converts it to angiotensin I. ACE (angiotensin converting enzyme) converts angiotensin I to angiotensin II. Angiotensin II raises blood pressure by constricting blood vessels. It triggers the release of aldosterone from the adrenal cortex, which in turn stimulates the renal tubules to reabsorb more sodium. Angiotensin II also triggers the release of anti-diuretic hormone from the hypothalamus, which leads to water retention. It acts directly on the nephrons and decreases GFR.
Glossary
- angiotensin II
- molecule that affects different organs to increase blood pressure
- angiotensin I
- product in the renin-angiotensin-aldosterone pathway
- angiotensin converting enzyme (ACE)
- enzyme that converts angiotensin I to angiotensin II
- anti-diuretic hormone (ADH)
- hormone that prevents the loss of water
- renin-angiotensin-aldosterone
- biochemical pathway that activates angiotensin II, which increases blood pressure
- vasodilator
- compound that increases the diameter of blood vessels
- vasopressin
- another name for anti-diuretic hormone
Attribution
This section is adapted from 22.5. Hormonal Control of Osmoregulatory Functions in Concepts of Biology – 1st Canadian Edition by Charles Molnar and Jane Gair which is licensed under a CC BY 4.0 License.
Learning Objectives
By the end of this section, you will be able to:
- Explain fetal development during the three trimesters of gestation
- Describe labor and delivery
- Compare the efficacy and duration of various types of contraception
- Discuss causes of infertility and the therapeutic options available
Pregnancy begins with the fertilization of an egg and continues through to the birth of the individual. The length of time of gestation varies among animals, but is very similar among the great apes: human gestation is 266 days, while chimpanzee gestation is 237 days, a gorilla’s is 257 days, and orangutan gestation is 260 days long. The fox has a 57-day gestation. Dogs and cats have similar gestations averaging 60 days. The longest gestation for a land mammal is an African elephant at 640 days. The longest gestations among marine mammals are the beluga and sperm whales at 460 days.
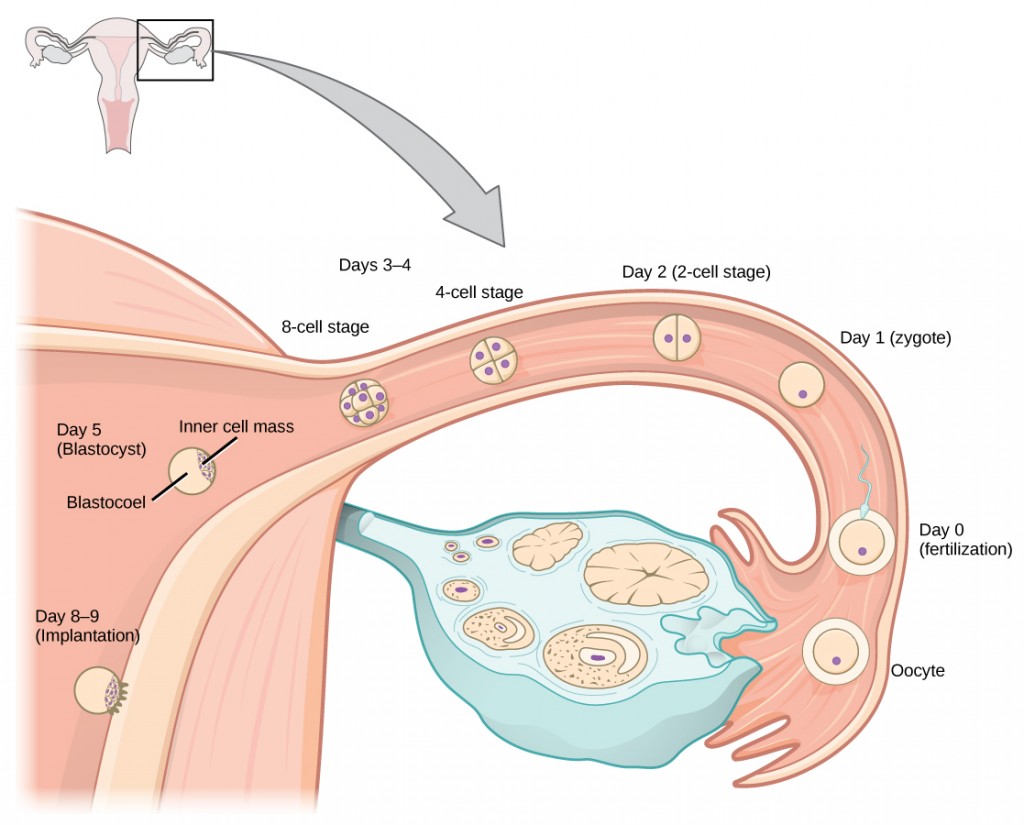
Human Gestation
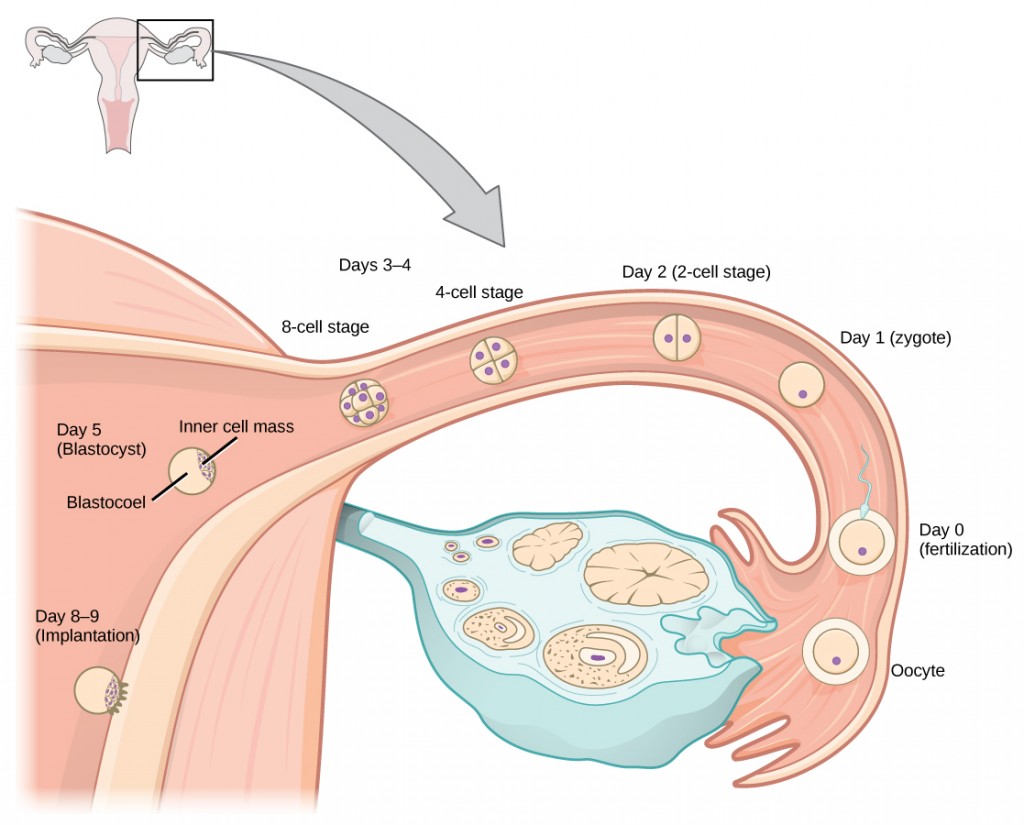
Twenty-four hours before fertilization, the egg has finished meiosis and becomes a mature oocyte. When fertilized (at conception) the egg becomes known as a zygote. The zygote travels through the oviduct to the uterus (Figure 24.18). The developing embryo must implant into the wall of the uterus within seven days, or it will deteriorate and die. The outer layers of the zygote (blastocyst) grow into the endometrium by digesting the endometrial cells, and wound healing of the endometrium closes up the blastocyst into the tissue. Another layer of the blastocyst, the chorion, begins releasing a hormone called human beta chorionic gonadotropin (β-HCG) which makes its way to the corpus luteum and keeps that structure active. This ensures adequate levels of progesterone that will maintain the endometrium of the uterus for the support of the developing embryo. Pregnancy tests determine the level of β-HCG in urine or serum. If the hormone is present, the test is positive.
The gestation period is divided into three equal periods or trimesters. During the first two to four weeks of the first trimester, nutrition and waste are handled by the endometrial lining through diffusion. As the trimester progresses, the outer layer of the embryo begins to merge with the endometrium, and the placenta forms. This organ takes over the nutrient and waste requirements of the embryo and fetus, with the mother’s blood passing nutrients to the placenta and removing waste from it. Chemicals from the fetus, such as bilirubin, are processed by the mother’s liver for elimination. Some of the mother’s immunoglobulins will pass through the placenta, providing passive immunity against some potential infections.
Internal organs and body structures begin to develop during the first trimester. By five weeks, limb buds, eyes, the heart, and liver have been basically formed. By eight weeks, the term fetus applies, and the body is essentially formed, as shown in Figure 24.19. The individual is about five centimeters (two inches) in length and many of the organs, such as the lungs and liver, are not yet functioning. Exposure to any toxins is especially dangerous during the first trimester, as all of the body’s organs and structures are going through initial development. Anything that affects that development can have a severe effect on the fetus’ survival.

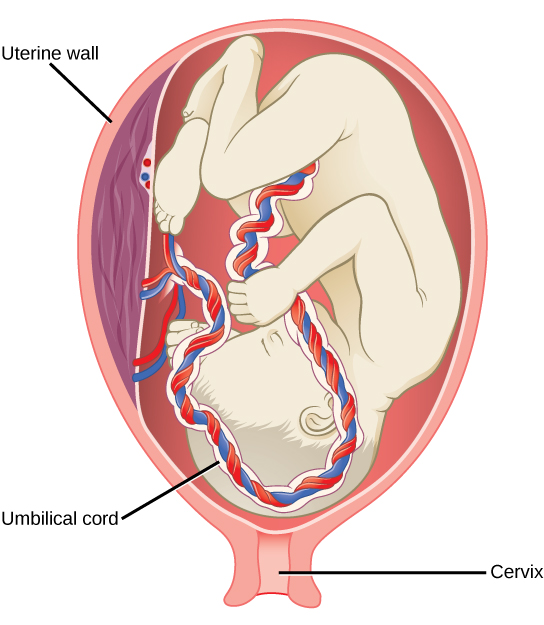
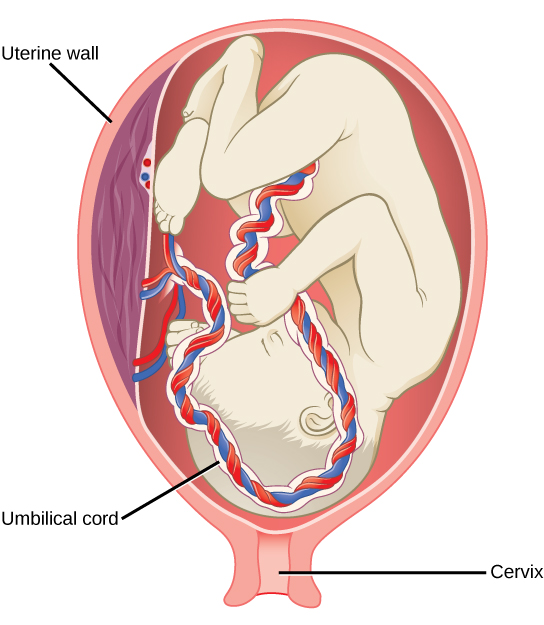
During the second trimester, the fetus grows to about 30 cm (12 inches), as shown in Figure 24.20. It becomes active and the mother usually feels the first movements. All organs and structures continue to develop. The placenta has taken over the functions of nutrition and waste and the production of estrogen and progesterone from the corpus luteum, which has degenerated. The placenta will continue functioning up through the delivery of the baby.

Concept in Action

Visit this site to see the stages of human fetal development.
Labor and Birth
Labor is the physical efforts of expulsion of the fetus and the placenta from the uterus during birth (parturition). Toward the end of the third trimester, estrogen causes receptors on the uterine wall to develop and bind the hormone oxytocin. At this time, the baby reorients, facing forward and down with the back or crown of the head engaging the cervix (uterine opening). This causes the cervix to stretch and nerve impulses are sent to the hypothalamus, which signals for the release of oxytocin from the posterior pituitary. The oxytocin causes the smooth muscle in the uterine wall to contract. At the same time, the placenta releases prostaglandins into the uterus, increasing the contractions. A positive feedback relay occurs between the uterus, hypothalamus, and the posterior pituitary to assure an adequate supply of oxytocin. As more smooth muscle cells are recruited, the contractions increase in intensity and force.
There are three stages to labor. During stage one, the cervix thins and dilates. This is necessary for the baby and placenta to be expelled during birth. The cervix will eventually dilate to about 10 cm. During stage two, the baby is expelled from the uterus. The uterus contracts and the mother pushes as she compresses her abdominal muscles to aid the delivery. The last stage is the passage of the placenta after the baby has been born and the organ has completely disengaged from the uterine wall. If labor should stop before stage two is reached, synthetic oxytocin, known as Pitocin, can be administered to restart and maintain labor.
An alternative to labor and delivery is the surgical delivery of the baby through a procedure called a Caesarian section. This is major abdominal surgery and can lead to post-surgical complications for the mother, but in some cases it may be the only way to safely deliver the baby.
The mother’s mammary glands go through changes during the third trimester to prepare for lactation and breastfeeding. When the baby begins suckling at the breast, signals are sent to the hypothalamus causing the release of prolactin from the anterior pituitary. Prolactin causes the mammary glands to produce milk. Oxytocin is also released, promoting the release of the milk. The milk contains nutrients for the baby’s development and growth as well as immunoglobulins to protect the child from bacterial and viral infections.
Contraception and Birth Control
The prevention of a pregnancy comes under the terms contraception or birth control. Strictly speaking, contraception refers to preventing the sperm and egg from joining. Both terms are, however, frequently used interchangeably.
| Method | Examples | Failure Rate in Typical Use Over 12 Months |
|---|---|---|
| Barrier | male condom, female condom, sponge, cervical cap, diaphragm, spermicides | 15 to 24% |
| Hormonal | oral, patch, vaginal ring | 8% |
| injection | 3% | |
| implant | less than 1% | |
| Other | natural family planning | 12 to 25% |
| withdrawal | 27% | |
| sterilization | less than 1% |
Table 24.3 lists common methods of contraception. The failure rates listed are not the ideal rates that could be realized, but the typical rates that occur. A failure rate is the number of pregnancies resulting from the method’s use over a twelve-month period. Barrier methods, such as condoms, cervical caps, and diaphragms, block sperm from entering the uterus, preventing fertilization. Spermicides are chemicals that are placed in the vagina that kill sperm. Sponges, which are saturated with spermicides, are placed in the vagina at the cervical opening. Combinations of spermicidal chemicals and barrier methods achieve lower failure rates than do the methods when used separately.
Nearly a quarter of the couples using barrier methods, natural family planning, or withdrawal can expect a failure of the method. Natural family planning is based on the monitoring of the menstrual cycle and having intercourse only during times when the egg is not available. A woman’s body temperature may rise a degree Celsius at ovulation and the cervical mucus may increase in volume and become more pliable. These changes give a general indication of when intercourse is more or less likely to result in fertilization. Withdrawal involves the removal of the penis from the vagina during intercourse, before ejaculation occurs. This is a risky method with a high failure rate due to the possible presence of sperm in the bulbourethral gland’s secretion, which may enter the vagina prior to removing the penis.
Hormonal methods use synthetic progesterone (sometimes in combination with estrogen), to inhibit the hypothalamus from releasing FSH or LH, and thus prevent an egg from being available for fertilization. The method of administering the hormone affects failure rate. The most reliable method, with a failure rate of less than 1 percent, is the implantation of the hormone under the skin. The same rate can be achieved through the sterilization procedures of vasectomy in the man or of tubal ligation in the woman, or by using an intrauterine device (IUD). IUDs are inserted into the uterus and establish an inflammatory condition that prevents fertilized eggs from implanting into the uterine wall.
Compliance with the contraceptive method is a strong contributor to the success or failure rate of any particular method. The only method that is completely effective at preventing conception is abstinence. The choice of contraceptive method depends on the goals of the woman or couple. Tubal ligation and vasectomy are considered permanent prevention, while other methods are reversible and provide short-term contraception.
Termination of an existing pregnancy can be spontaneous or voluntary. Spontaneous termination is a miscarriage and usually occurs very early in the pregnancy, usually within the first few weeks. This occurs when the fetus cannot develop properly and the gestation is naturally terminated. Voluntary termination of a pregnancy is an abortion. Laws regulating abortion vary between states and tend to view fetal viability as the criteria for allowing or preventing the procedure.
Infertility
Infertility is the inability to conceive a child or carry a child to birth. About 75 percent of causes of infertility can be identified; these include diseases, such as sexually transmitted diseases that can cause scarring of the reproductive tubes in either men or women, or developmental problems frequently related to abnormal hormone levels in one of the individuals. Inadequate nutrition, especially starvation, can delay menstruation. Stress can also lead to infertility. Short-term stress can affect hormone levels, while long-term stress can delay puberty and cause less frequent menstrual cycles. Other factors that affect fertility include toxins (such as cadmium), tobacco smoking, marijuana use, gonadal injuries, and aging.
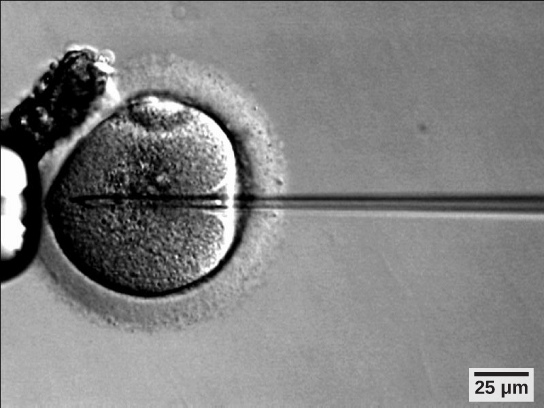
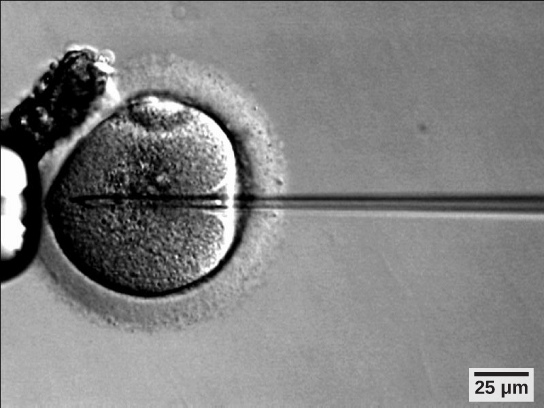
If infertility is identified, several assisted reproductive technologies (ART) are available to aid conception. A common type of ART is in vitro fertilization (IVF) where an egg and sperm are combined outside the body and then placed in the uterus. Eggs are obtained from the woman after extensive hormonal treatments that prepare mature eggs for fertilization and prepare the uterus for implantation of the fertilized egg. Sperm are obtained from the man and they are combined with the eggs and supported through several cell divisions to ensure viability of the zygotes. When the embryos have reached the eight-cell stage, one or more is implanted into the woman’s uterus. If fertilization is not accomplished by simple IVF, a procedure that injects the sperm into an egg can be used. This is called intracytoplasmic sperm injection (ICSI) and is shown in Figure 24.22. IVF procedures produce a surplus of fertilized eggs and embryos that can be frozen and stored for future use. The procedures can also result in multiple births.
Summary
Human pregnancy begins with fertilization of an egg and proceeds through the three trimesters of gestation. The labor process has three stages (contractions, delivery of the fetus, expulsion of the placenta), each propelled by hormones. The first trimester lays down the basic structures of the body, including the limb buds, heart, eyes, and the liver. The second trimester continues the development of all of the organs and systems. The third trimester exhibits the greatest growth of the fetus and culminates in labor and delivery. Prevention of a pregnancy can be accomplished through a variety of methods including barriers, hormones, or other means. Assisted reproductive technologies may help individuals who have infertility problems.
Exercises
- Nutrient and waste requirements for the developing fetus are handled during the first few weeks by:
- the placenta
- diffusion through the endometrium
- the chorion
- the blastocyst
- Progesterone is made during the third trimester by the:
- placenta
- endometrial lining
- chorion
- corpus luteum
- Which contraceptive method is 100 percent effective at preventing pregnancy?
- condom
- oral hormonal methods
- sterilization
- abstinence
- Which type of short term contraceptive method is generally more effective than others?
- barrier
- horomonal
- natural family planning
- withdrawal
- Which hormone is primarily responsible for the contractions during labor?
- oxytocin
- estrogen
- β-HCG
- progesterone
- Major organs begin to develop during which part of human gestation?
- fertilization
- first trimester
- second trimester
- third trimester
- Describe the major developments during each trimester of human gestation.
- Describe the stages of labor.
Answers
- B
- A
- D
- B
- A
- B
- The first trimester lays down the basic structures of the body, including the limb buds, heart, eyes, and the liver. The second trimester continues the development of all of the organs and systems established during the first trimester. The placenta takes over the production of estrogen and high levels of progesterone and handles the nutrient and waste requirements of the fetus. The third trimester exhibits the greatest growth of the fetus, culminating in labor and delivery.
- Stage one of labor results in the thinning of the cervix and the dilation of the cervical opening. Stage two delivers the baby, and stage three delivers the placenta.
Glossary
contraception (also, birth control)
various means used to prevent pregnancy
gestation
length of time for fetal development to birth
human beta chorionic gonadotropin (β-HCG)
hormone produced by the chorion of the zygote that helps to maintain the corpus luteum and elevated levels of progesterone
infertility
inability to conceive, carry, and deliver children
placenta
organ that supports the diffusion of nutrients and waste between the mother’s and fetus’ blood
Learning Objectives
By the end of this section, you will be able to:
- Explain fetal development during the three trimesters of gestation
- Describe labor and delivery
- Compare the efficacy and duration of various types of contraception
- Discuss causes of infertility and the therapeutic options available
Pregnancy begins with the fertilization of an egg and continues through to the birth of the individual. The length of time of gestation varies among animals, but is very similar among the great apes: human gestation is 266 days, while chimpanzee gestation is 237 days, a gorilla’s is 257 days, and orangutan gestation is 260 days long. The fox has a 57-day gestation. Dogs and cats have similar gestations averaging 60 days. The longest gestation for a land mammal is an African elephant at 640 days. The longest gestations among marine mammals are the beluga and sperm whales at 460 days.
Human Gestation
Twenty-four hours before fertilization, the egg has finished meiosis and becomes a mature oocyte. When fertilized (at conception) the egg becomes known as a zygote. The zygote travels through the oviduct to the uterus (Figure 24.18). The developing embryo must implant into the wall of the uterus within seven days, or it will deteriorate and die. The outer layers of the zygote (blastocyst) grow into the endometrium by digesting the endometrial cells, and wound healing of the endometrium closes up the blastocyst into the tissue. Another layer of the blastocyst, the chorion, begins releasing a hormone called human beta chorionic gonadotropin (β-HCG) which makes its way to the corpus luteum and keeps that structure active. This ensures adequate levels of progesterone that will maintain the endometrium of the uterus for the support of the developing embryo. Pregnancy tests determine the level of β-HCG in urine or serum. If the hormone is present, the test is positive.
The gestation period is divided into three equal periods or trimesters. During the first two to four weeks of the first trimester, nutrition and waste are handled by the endometrial lining through diffusion. As the trimester progresses, the outer layer of the embryo begins to merge with the endometrium, and the placenta forms. This organ takes over the nutrient and waste requirements of the embryo and fetus, with the mother’s blood passing nutrients to the placenta and removing waste from it. Chemicals from the fetus, such as bilirubin, are processed by the mother’s liver for elimination. Some of the mother’s immunoglobulins will pass through the placenta, providing passive immunity against some potential infections.
Internal organs and body structures begin to develop during the first trimester. By five weeks, limb buds, eyes, the heart, and liver have been basically formed. By eight weeks, the term fetus applies, and the body is essentially formed, as shown in Figure 24.19. The individual is about five centimeters (two inches) in length and many of the organs, such as the lungs and liver, are not yet functioning. Exposure to any toxins is especially dangerous during the first trimester, as all of the body’s organs and structures are going through initial development. Anything that affects that development can have a severe effect on the fetus’ survival.

During the second trimester, the fetus grows to about 30 cm (12 inches), as shown in Figure 24.20. It becomes active and the mother usually feels the first movements. All organs and structures continue to develop. The placenta has taken over the functions of nutrition and waste and the production of estrogen and progesterone from the corpus luteum, which has degenerated. The placenta will continue functioning up through the delivery of the baby.

Concept in Action

Visit this site to see the stages of human fetal development.
Labor and Birth
Labor is the physical efforts of expulsion of the fetus and the placenta from the uterus during birth (parturition). Toward the end of the third trimester, estrogen causes receptors on the uterine wall to develop and bind the hormone oxytocin. At this time, the baby reorients, facing forward and down with the back or crown of the head engaging the cervix (uterine opening). This causes the cervix to stretch and nerve impulses are sent to the hypothalamus, which signals for the release of oxytocin from the posterior pituitary. The oxytocin causes the smooth muscle in the uterine wall to contract. At the same time, the placenta releases prostaglandins into the uterus, increasing the contractions. A positive feedback relay occurs between the uterus, hypothalamus, and the posterior pituitary to assure an adequate supply of oxytocin. As more smooth muscle cells are recruited, the contractions increase in intensity and force.
There are three stages to labor. During stage one, the cervix thins and dilates. This is necessary for the baby and placenta to be expelled during birth. The cervix will eventually dilate to about 10 cm. During stage two, the baby is expelled from the uterus. The uterus contracts and the mother pushes as she compresses her abdominal muscles to aid the delivery. The last stage is the passage of the placenta after the baby has been born and the organ has completely disengaged from the uterine wall. If labor should stop before stage two is reached, synthetic oxytocin, known as Pitocin, can be administered to restart and maintain labor.
An alternative to labor and delivery is the surgical delivery of the baby through a procedure called a Caesarian section. This is major abdominal surgery and can lead to post-surgical complications for the mother, but in some cases it may be the only way to safely deliver the baby.
The mother’s mammary glands go through changes during the third trimester to prepare for lactation and breastfeeding. When the baby begins suckling at the breast, signals are sent to the hypothalamus causing the release of prolactin from the anterior pituitary. Prolactin causes the mammary glands to produce milk. Oxytocin is also released, promoting the release of the milk. The milk contains nutrients for the baby’s development and growth as well as immunoglobulins to protect the child from bacterial and viral infections.
Contraception and Birth Control
The prevention of a pregnancy comes under the terms contraception or birth control. Strictly speaking, contraception refers to preventing the sperm and egg from joining. Both terms are, however, frequently used interchangeably.
| Method | Examples | Failure Rate in Typical Use Over 12 Months |
|---|---|---|
| Barrier | male condom, female condom, sponge, cervical cap, diaphragm, spermicides | 15 to 24% |
| Hormonal | oral, patch, vaginal ring | 8% |
| injection | 3% | |
| implant | less than 1% | |
| Other | natural family planning | 12 to 25% |
| withdrawal | 27% | |
| sterilization | less than 1% |
Table 24.3 lists common methods of contraception. The failure rates listed are not the ideal rates that could be realized, but the typical rates that occur. A failure rate is the number of pregnancies resulting from the method’s use over a twelve-month period. Barrier methods, such as condoms, cervical caps, and diaphragms, block sperm from entering the uterus, preventing fertilization. Spermicides are chemicals that are placed in the vagina that kill sperm. Sponges, which are saturated with spermicides, are placed in the vagina at the cervical opening. Combinations of spermicidal chemicals and barrier methods achieve lower failure rates than do the methods when used separately.
Nearly a quarter of the couples using barrier methods, natural family planning, or withdrawal can expect a failure of the method. Natural family planning is based on the monitoring of the menstrual cycle and having intercourse only during times when the egg is not available. A woman’s body temperature may rise a degree Celsius at ovulation and the cervical mucus may increase in volume and become more pliable. These changes give a general indication of when intercourse is more or less likely to result in fertilization. Withdrawal involves the removal of the penis from the vagina during intercourse, before ejaculation occurs. This is a risky method with a high failure rate due to the possible presence of sperm in the bulbourethral gland’s secretion, which may enter the vagina prior to removing the penis.
Hormonal methods use synthetic progesterone (sometimes in combination with estrogen), to inhibit the hypothalamus from releasing FSH or LH, and thus prevent an egg from being available for fertilization. The method of administering the hormone affects failure rate. The most reliable method, with a failure rate of less than 1 percent, is the implantation of the hormone under the skin. The same rate can be achieved through the sterilization procedures of vasectomy in the man or of tubal ligation in the woman, or by using an intrauterine device (IUD). IUDs are inserted into the uterus and establish an inflammatory condition that prevents fertilized eggs from implanting into the uterine wall.
Compliance with the contraceptive method is a strong contributor to the success or failure rate of any particular method. The only method that is completely effective at preventing conception is abstinence. The choice of contraceptive method depends on the goals of the woman or couple. Tubal ligation and vasectomy are considered permanent prevention, while other methods are reversible and provide short-term contraception.
Termination of an existing pregnancy can be spontaneous or voluntary. Spontaneous termination is a miscarriage and usually occurs very early in the pregnancy, usually within the first few weeks. This occurs when the fetus cannot develop properly and the gestation is naturally terminated. Voluntary termination of a pregnancy is an abortion. Laws regulating abortion vary between states and tend to view fetal viability as the criteria for allowing or preventing the procedure.
Infertility
Infertility is the inability to conceive a child or carry a child to birth. About 75 percent of causes of infertility can be identified; these include diseases, such as sexually transmitted diseases that can cause scarring of the reproductive tubes in either men or women, or developmental problems frequently related to abnormal hormone levels in one of the individuals. Inadequate nutrition, especially starvation, can delay menstruation. Stress can also lead to infertility. Short-term stress can affect hormone levels, while long-term stress can delay puberty and cause less frequent menstrual cycles. Other factors that affect fertility include toxins (such as cadmium), tobacco smoking, marijuana use, gonadal injuries, and aging.
If infertility is identified, several assisted reproductive technologies (ART) are available to aid conception. A common type of ART is in vitro fertilization (IVF) where an egg and sperm are combined outside the body and then placed in the uterus. Eggs are obtained from the woman after extensive hormonal treatments that prepare mature eggs for fertilization and prepare the uterus for implantation of the fertilized egg. Sperm are obtained from the man and they are combined with the eggs and supported through several cell divisions to ensure viability of the zygotes. When the embryos have reached the eight-cell stage, one or more is implanted into the woman’s uterus. If fertilization is not accomplished by simple IVF, a procedure that injects the sperm into an egg can be used. This is called intracytoplasmic sperm injection (ICSI) and is shown in Figure 24.22. IVF procedures produce a surplus of fertilized eggs and embryos that can be frozen and stored for future use. The procedures can also result in multiple births.
Summary
Human pregnancy begins with fertilization of an egg and proceeds through the three trimesters of gestation. The labor process has three stages (contractions, delivery of the fetus, expulsion of the placenta), each propelled by hormones. The first trimester lays down the basic structures of the body, including the limb buds, heart, eyes, and the liver. The second trimester continues the development of all of the organs and systems. The third trimester exhibits the greatest growth of the fetus and culminates in labor and delivery. Prevention of a pregnancy can be accomplished through a variety of methods including barriers, hormones, or other means. Assisted reproductive technologies may help individuals who have infertility problems.
Exercises
- Nutrient and waste requirements for the developing fetus are handled during the first few weeks by:
- the placenta
- diffusion through the endometrium
- the chorion
- the blastocyst
- Progesterone is made during the third trimester by the:
- placenta
- endometrial lining
- chorion
- corpus luteum
- Which contraceptive method is 100 percent effective at preventing pregnancy?
- condom
- oral hormonal methods
- sterilization
- abstinence
- Which type of short term contraceptive method is generally more effective than others?
- barrier
- horomonal
- natural family planning
- withdrawal
- Which hormone is primarily responsible for the contractions during labor?
- oxytocin
- estrogen
- β-HCG
- progesterone
- Major organs begin to develop during which part of human gestation?
- fertilization
- first trimester
- second trimester
- third trimester
- Describe the major developments during each trimester of human gestation.
- Describe the stages of labor.
Answers
- B
- A
- D
- B
- A
- B
- The first trimester lays down the basic structures of the body, including the limb buds, heart, eyes, and the liver. The second trimester continues the development of all of the organs and systems established during the first trimester. The placenta takes over the production of estrogen and high levels of progesterone and handles the nutrient and waste requirements of the fetus. The third trimester exhibits the greatest growth of the fetus, culminating in labor and delivery.
- Stage one of labor results in the thinning of the cervix and the dilation of the cervical opening. Stage two delivers the baby, and stage three delivers the placenta.
Glossary
contraception (also, birth control)
various means used to prevent pregnancy
gestation
length of time for fetal development to birth
human beta chorionic gonadotropin (β-HCG)
hormone produced by the chorion of the zygote that helps to maintain the corpus luteum and elevated levels of progesterone
infertility
inability to conceive, carry, and deliver children
placenta
organ that supports the diffusion of nutrients and waste between the mother’s and fetus’ blood