32 Spinal Motor Control and Proprioception
The motor system refers to the nerve cells that are used to control our body. The key roles of the motor system are to plan, control, and execute voluntary (deliberate) movements, and to control involuntary (subconscious or automatic) functions, such as digesting food. The motor system is sometimes described as a top-down process: in a voluntary movement, neural activity in the frontal lobe sends commands down to motor neurons located in the brainstem or spinal cord, which in turn activate muscle groups. In reality, motor control is more of a loop, rapidly communicating between the sensory cortex and motor cortex. Sensory information about limb position, posture, and objects in contact with the skin inform the descending motor plan. Simultaneously, the motor plan provides predictions about upcoming movement.
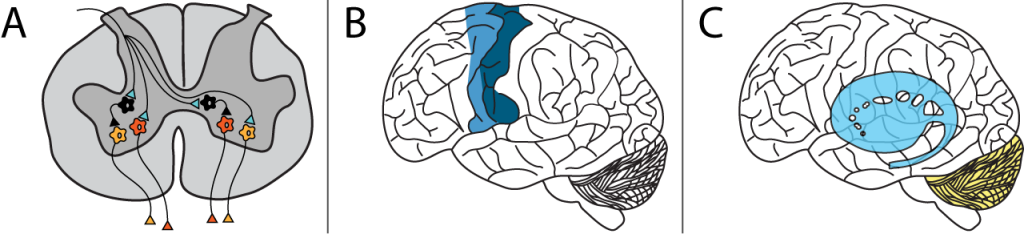
There are multiple levels of control. Within the spinal cord, simple reflexes can function without higher input from the brain. Slightly more complex spinal control occurs when central pattern generators function during repetitive movements like walking. The motor and premotor cortices in the brain are responsible for the planning and execution of voluntary movements. And finally, the basal ganglia and cerebellum modulate the responses of the neurons in the motor cortex to help with coordination, motor learning, and balance.
This lesson explores the lowest level of control at the level of the spinal cord.
Alpha Motor Neurons
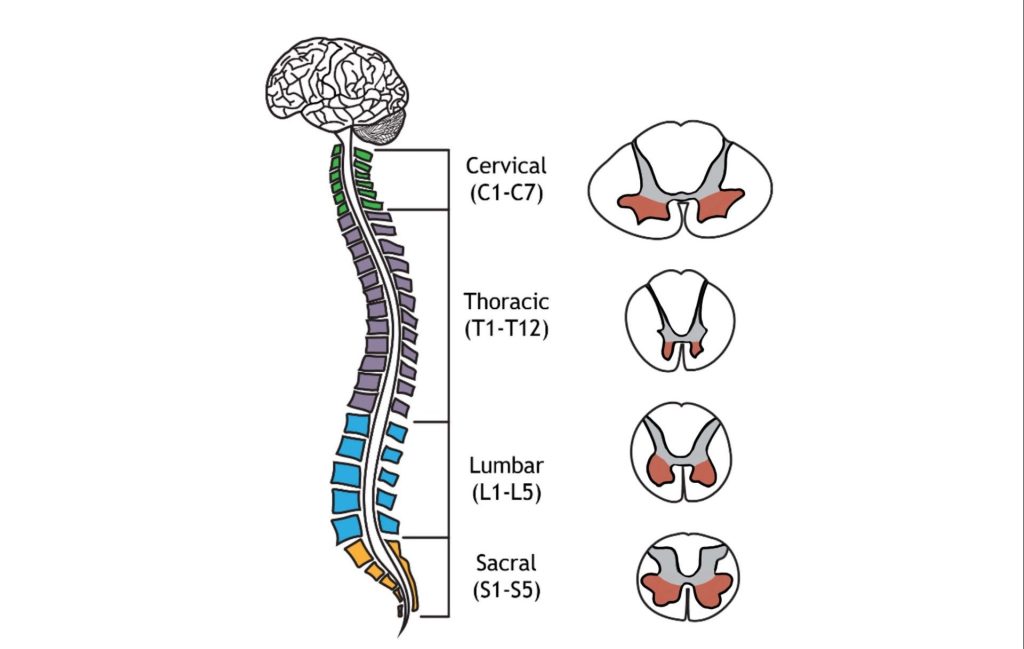
Muscle fibers are innervated by alpha motor neurons. Alpha motor neurons are also called lower motor neurons because they are not located in higher brain areas. These cells are the only cells that directly command muscle contraction. The cell bodies of the alpha motor neurons are located in the central nervous system in the ventral horn of the spinal cord. Their axons leave the spinal cord via the ventral roots and travel to the muscle via efferent peripheral spinal nerves.
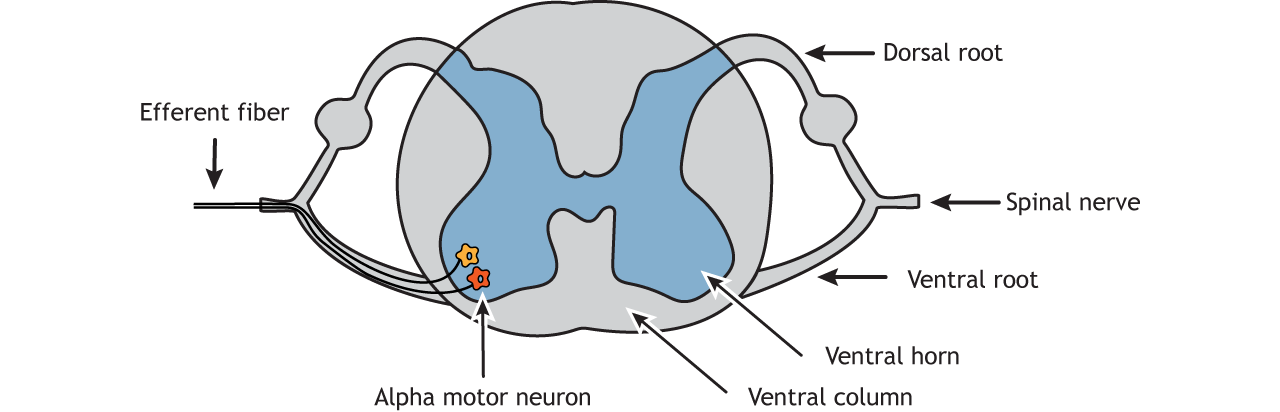
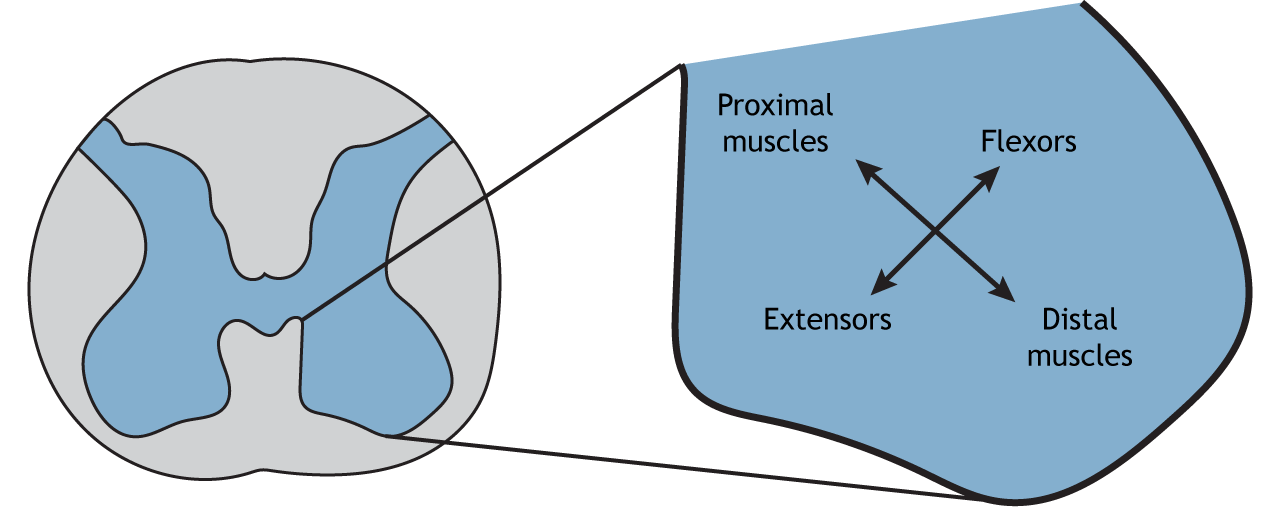
Like the sensory systems, the motor system is also organized in a topographic fashion, referred to as ‘somatotopic organization’. Within the spinal cord, alpha motor neurons that innervate muscles in the arms and legs are located in the lateral portion of the ventral horn, whereas alpha motor neurons that innervate muscles in the trunk are located in the medial portion.
Location of Alpha Motor Neurons
The structure of the spinal cord is reviewed in Chapter 21. Examining cross sections of the spinal cord at different levels reveals that there is a non-uniform distribution of lower motor neurons. This is determined by the size of the ventral horn at the different levels of the spinal cord. At the cervical enlargement the larger ventral horns are due to the presence of more lower motor neurons that function in movement of the arms. At the lumbar enlargement the larger ventral horns are due to the presence of more lower motor neurons that function in movement of the legs.
Neuromuscular Junction
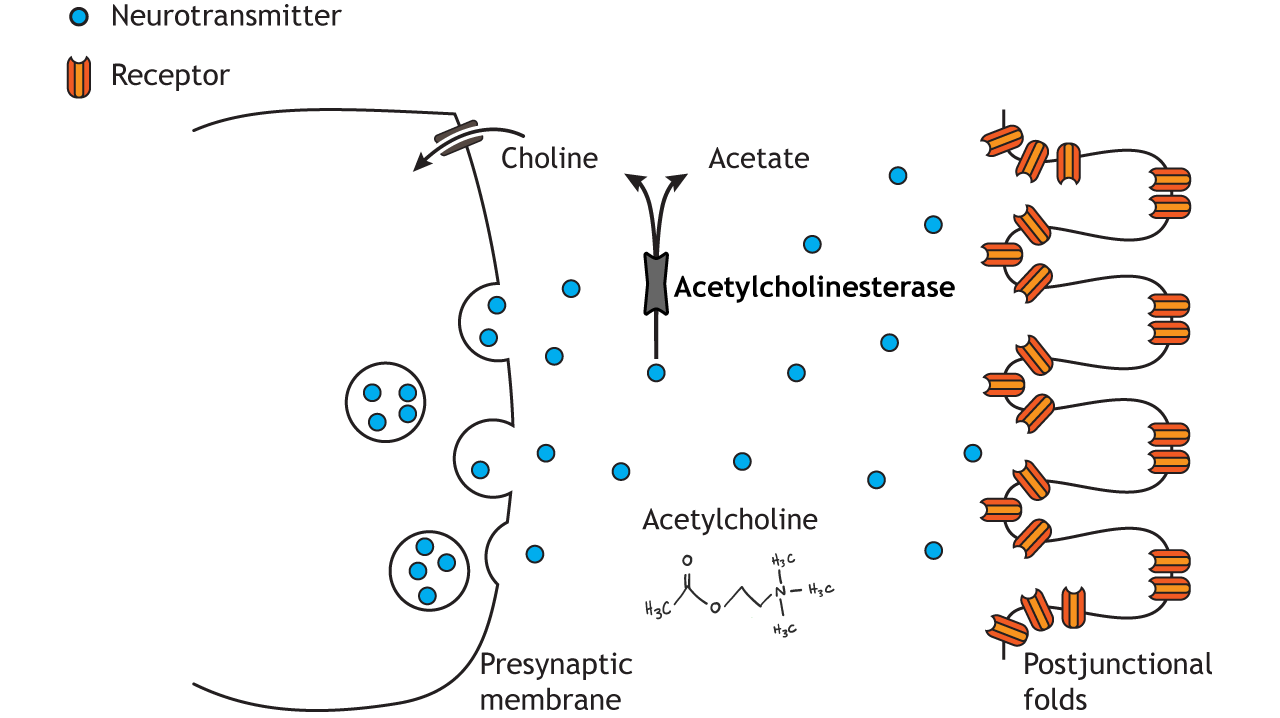
The lower motor neurons communicate with muscle fibers (muscle cells) at the neuromuscular junction (NMJ). The NMJ is similar to other chemical synapses, however the postsynaptic cell is a muscle cell separated by about 30 nm. The presynaptic cell is the motor neuron and the postsynaptic site is the sarcolemma, the cell membrane of the long cylindrical muscle fibers (muscle cells). The neuromuscular junction is one of the largest synapses in the body and one of the most well-studied because of its peripheral location.
The neuromuscular junction is located midway down the length of the muscle fiber. The muscle fiber will contract in response to depolarization traveling down the sarcolemma of the muscle fiber. The synapse is located midway down the length of the muscle fiber so that the postsynaptic signal can travel in both directions down the long muscle fiber and quickly activate a contraction along the entire cell.
Acetylcholine is the neurotransmitter released at the neuromuscular junction (NMJ), and it acts upon ligand-gated, non-selective cation channels called nicotinic acetylcholine receptors that are present in postjunctional folds of the muscle fiber. Nicotinic acetylcholine receptors allow the influx of sodium ions into the muscle cell. The depolarization will cause nearby voltage-gated channels to open and fire an action potential in the muscle fiber. In a healthy system, an action potential in the motor neurons always causes an action potential in the muscle cell. The action potential leads to contraction of the muscle fiber.
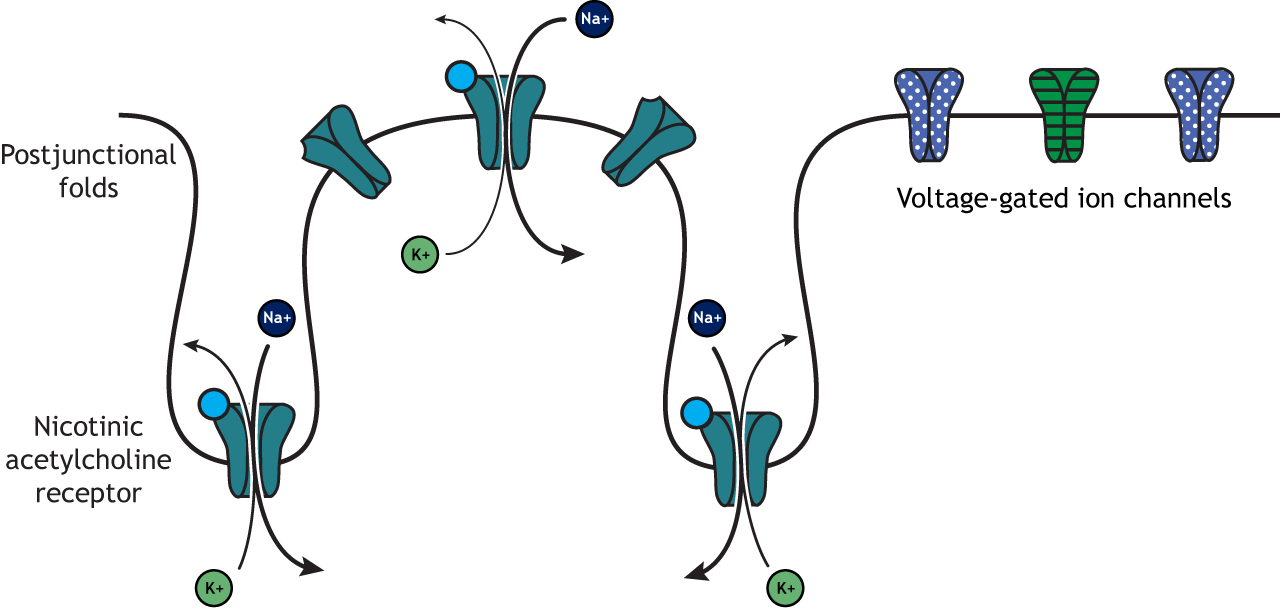
To review, an action potential traveling down the motor neuron (presynaptic cell) will cause the release of acetylcholine into the synapse. Acetylcholine binds to postsynaptic nicotinic acetylcholine receptors that are located in the folded sarcolemma (increasing surface area), causing depolarization of muscle fibers and ultimately muscle contraction.
Acetylcholinesterase, an enzyme that breaks down acetylcholine and terminates its action, is present in the synaptic cleft of the neuromuscular junction. Muscle contraction must be tightly controlled. Thus, the actions of acetylcholinesterase are very important to cease muscle contraction quickly.
Clinical Application: Myasthenia gravis
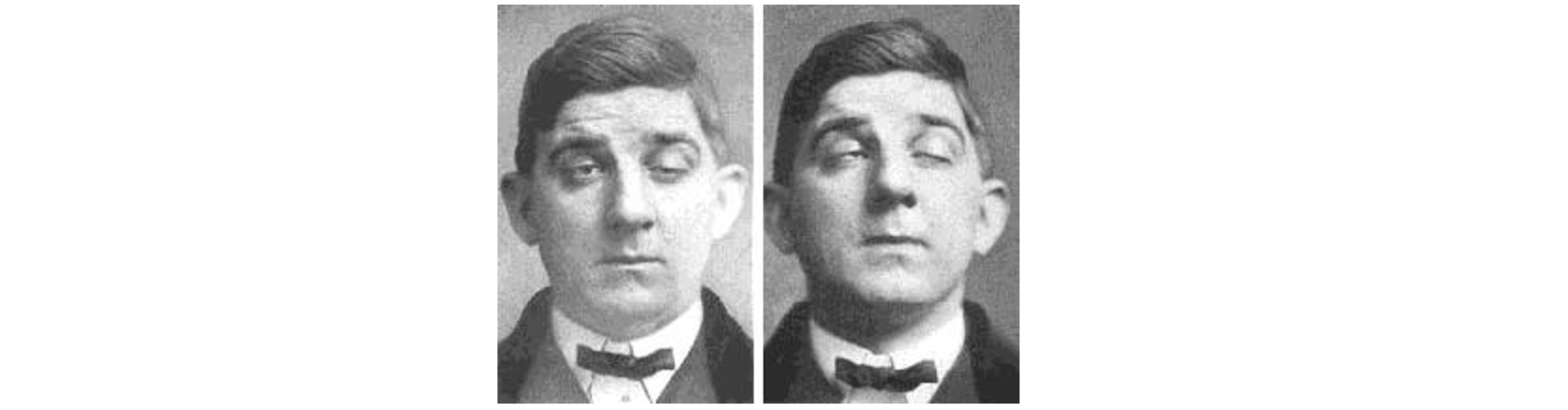
Myasthenia gravis (MG) is an autoimmune disorder characterized by muscle weakness, resulting in difficulty with speech, trouble with movement and swallowing, drooping eyelids, and double vision. Each year, an estimated 20 out of a million people get diagnosed with MG.
The muscle weakness seen in MG results from immune system-mediated destruction of the nicotinic acetylcholine receptors expressed at the NMJ. Thus, when the lower motor neuron releases acetylcholine, the muscle cells are unable to detect this release, so they fail to contract appropriately.
One therapeutic strategy involves inhibition of acetylcholinesterase, the enzyme that degrades acetylcholine. This causes the synaptic acetylcholine to remain in the synapse longer, increasing the chance that receptors get activated. Alternatively, autoimmune diseases like MG can be improved with immunosuppressant therapy. With successful treatment, MG usually does not result in changes in lifespan.
Motor Units
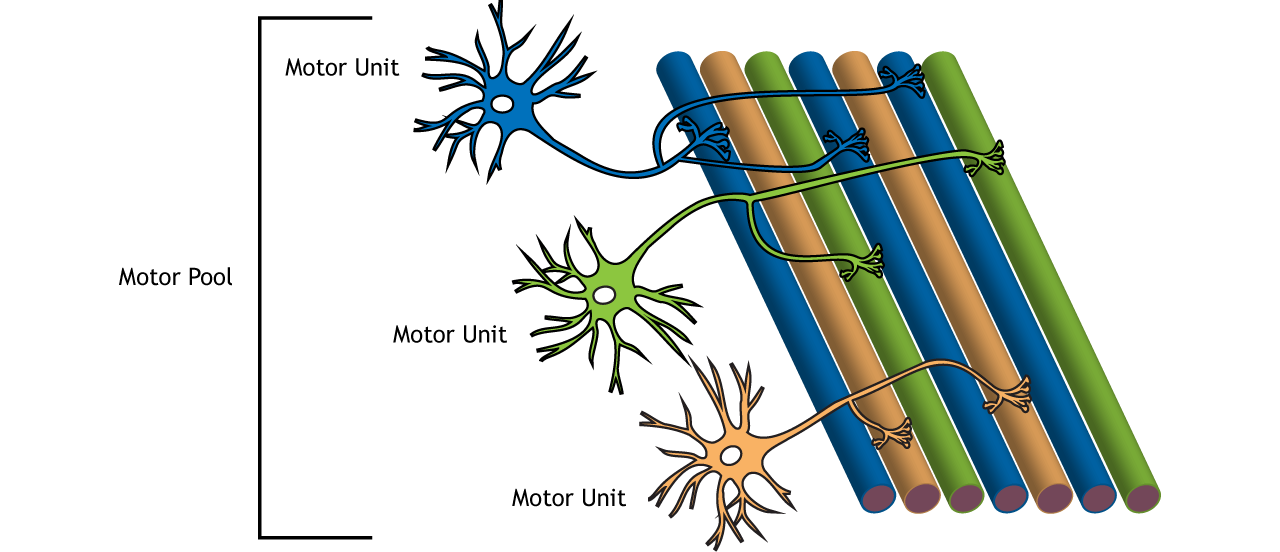
Importantly, there are many more muscles cells than there are motor neurons. One alpha motor neuron can innervate multiple fibers within one muscle due to the branching of motor neuron axons. Each axon terminal synapses (innervates) a single muscle fiber. A motor neuron and all the fibers innervated by it are called a motor unit. The muscle fibers within one motor unit are often spread throughout the muscle to spread the contraction throughout the full muscle. Further, motor units in a muscle usually contract asynchronously to help protect the muscle from fatigue. A graded contraction of the muscle is produced by activating varying numbers of motor units.
Motor units differ in size. Small motor units are motor units that innervate fewer muscle fibers and thus control fine movements. Small motor units are located in the eyes and fingers, both of which function in fine and precise movements. Large motor units innervate many muscle fibers and are typically found in weight-bearing muscles like the thighs.
The group of motor neurons that innervate all the fibers of one muscle is called a motor pool.
Types of Motor Units
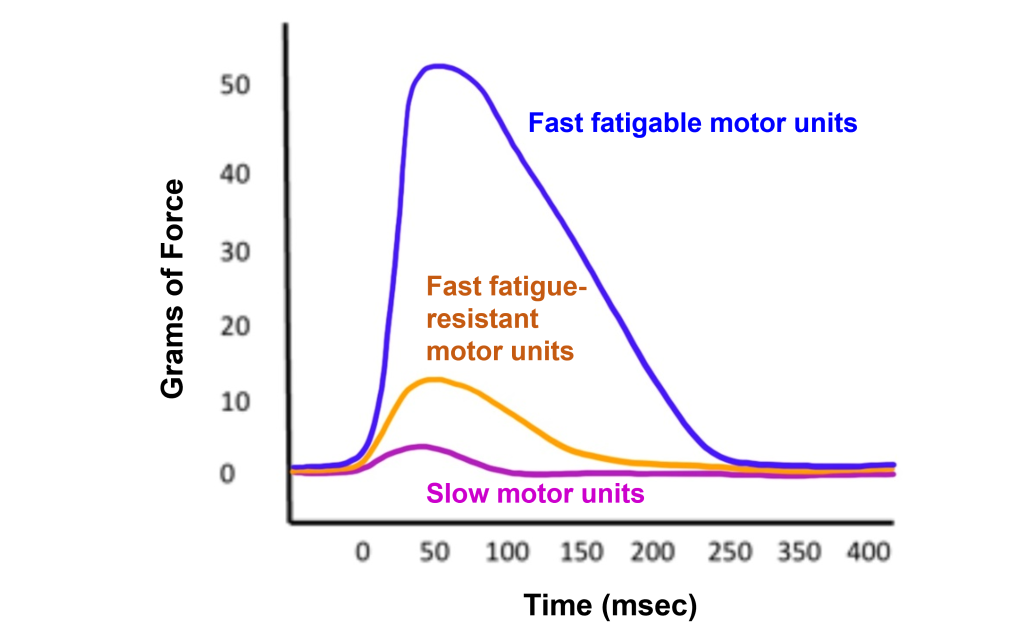
In addition to the size of the motor unit, the types of muscle fibers that are innervated by motor units can also differ. There are three different types of motor units:
- Slow motor units. Slow motor units are slow to contract and generate less force but can work for a long time. They are used in endurance exercise like jogging.
- Fast fatigue-resistant motor units. Fast fatigue-resistant motor units are quick to contract (though not as fast the fast fatigable motor units). These motor units generate more force that then slow motor units, but are much more resistant to fatigue than the fast fatigable motor units.
- Fast fatigable motor units. Fast fatigable motor units are quickest to contract and generate the most force. These motor units are more prone to fatigue due to decreased number of mitochondria within the muscles. Fast fatigable motor units generate a lot of force quickly, but also tire quickly. They are used mostly in high intensity exercise like lifting weights and sprinting.
Muscle Activation
Action Potential Triggered in a Muscle
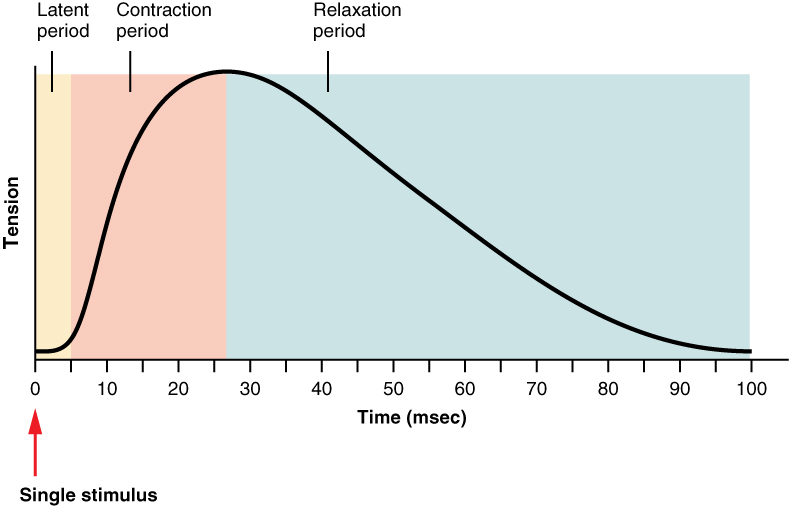
When an action potential is triggered in a muscle it causes a muscle twitch (contraction) that is followed by a period of relaxation. A muscle twitch shows an increase in tension after a short delay (latent period). During the contraction period, the muscle tension increased, and then has a long relaxation period, causing the muscle tension to be increased long after the initial stimulus.
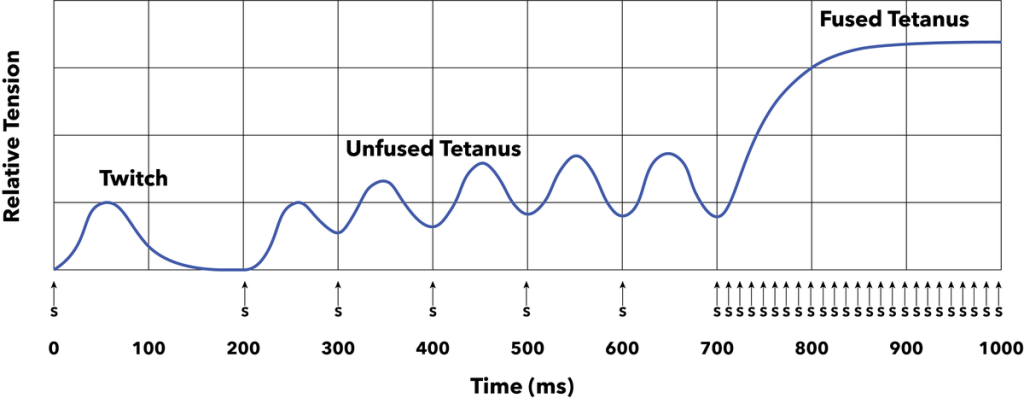
When a stimulus occurs during the relaxation period following one muscle twitch, the newly generated twitch will sum with the preceding one to increase the strength of the overall muscle contraction. Shortening the time between successive stimuli will result in unfused tetanus leading to a stronger contraction. Finally if stimuli are even closer together, a fused tetanus results. Thus, a higher rate of firing of the alpha motor neuron will generate more muscle contraction.
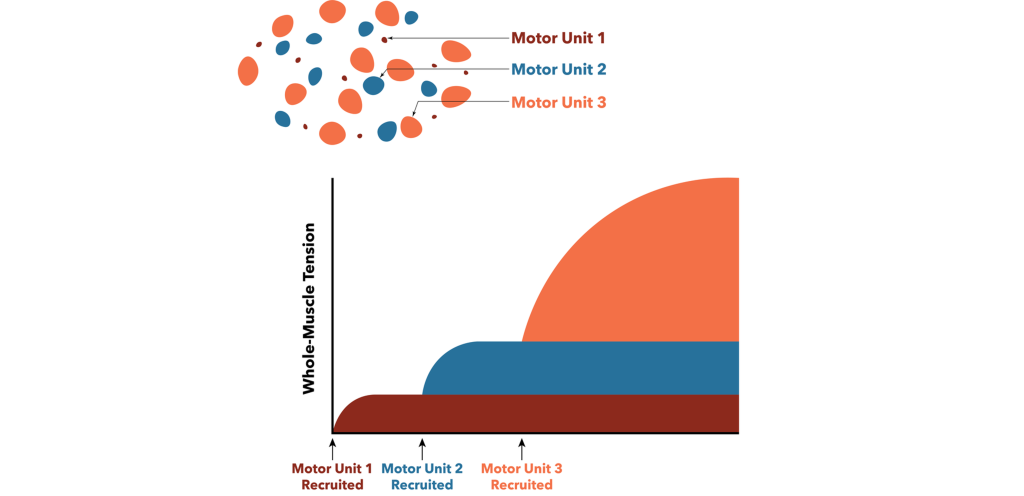
Muscle Recruitment
In addition to the rate of action potentials changing the force of the muscle contraction, muscle recruitment can also increase the strength of contraction within a muscle. When generating motor activity, the smallest motor units will be activated to contract first due to their size and increased excitability to move the load. Increasingly larger motor units are recruited to lift heavier loads. Recruitment of motor units allows for us to generate appropriate muscle tension to move a given load. For example, if you need to pick up a pencil, then we do not need to use the same force as if we were trying to pick up a 20-pound weight. Only smaller motor units would be activated to pick up the pencil, and increasingly larger motor units would be recruited to lift the heavier load of the 20-pound weight.
Alpha Motor Neuron Inputs
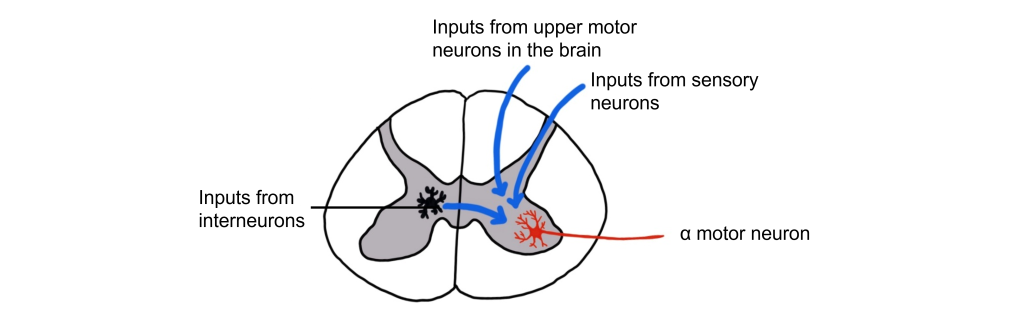
The alpha motor neurons that directly cause muscle contraction receive inputs from three different sources.
- Sensory cells from the dorsal root ganglion that provide sensory information from the muscles through proprioception.
- Upper motor neurons from the motor cortex in the brain and brain stem that are responsible for initiating voluntary movement.
- Interneurons in the spinal cord. These represent the largest input to the alpha motor neurons and can either provide excitation or inhibition to the alpha motor neuron.
Proprioception
Raise your arms above your head. Even without seeing your arms, your nervous system has mechanisms that inform you about the location and position of your body parts, including how much your joints are bent. This sense is called proprioception and is critically important for coordinated movement and motor reflexes that contribute to those tiny, rapid adjustments that are made while maintaining balance. Proprioceptive information ascends through the spinal cord and into the brain via the dorsal column-medial lemniscus tract. Proprioception is also processed in the primary somatosensory cortex.
Proprioception refers to the “body sense” that informs us about how our bodies are positioned and moving in space. Proprioceptors are receptors that provide proprioception information.
There are two main types of proprioceptors:
- Muscle spindles measure muscle stretch (muscle length) and transmit this sensory information via 1a sensory afferent fibers. Muscle spindles are nested within and arranged parallel to the extrafusal muscle fibers.
- Golgi Tendon Organs measure muscle tension and transmit this sensory information via 1b sensory afferent fibers. Golgi tendon organs are located between the extrafusal muscle fibers and their points of attachment at the bone.
Muscle Spindles
Extrafusal and Intrafusal Muscle Fibers
Muscle spindles are fibrous capsules that are located within muscles. Intrafusal muscle fibers are special muscle fibers that are located within the fibrous capsule of the muscle spindle. The intrafusal muscle fibers are innervated by gamma motor neurons that will cause them to contract.
Extrafusal muscle fibers, however, make up the bulk of the muscle and are located outside of the muscle spindle. The extrafusal muscle fibers are stimulated to contract by the alpha motor neurons.
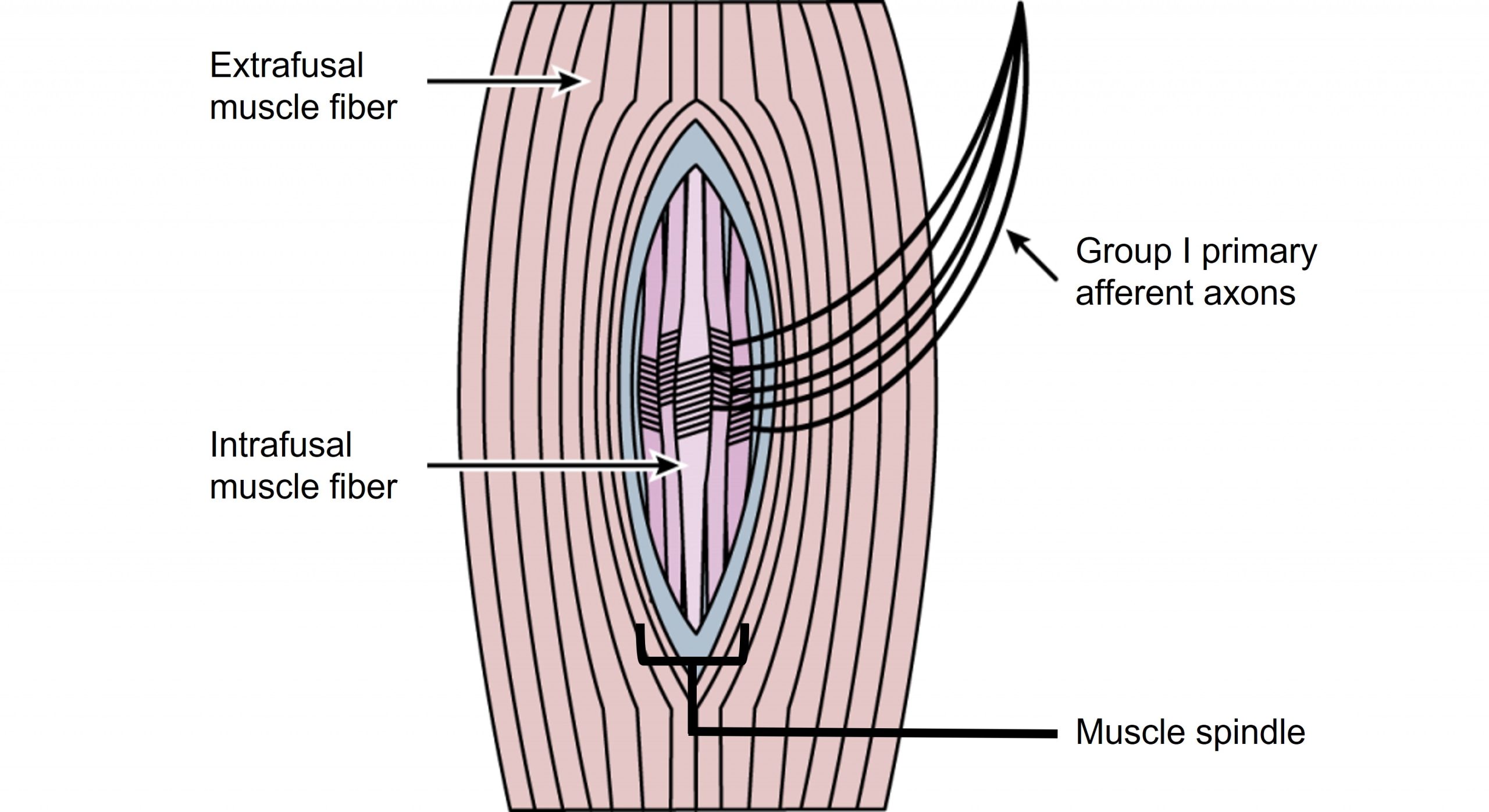
Muscle Spindles Function
Group 1a sensory afferent axons, which have a large diameter and are heavily myelinated, wrap around the intrafusal fibers contained within the muscle spindle. These sensory afferent fibers will signal when the intrafusal fibers of the muscle spindle are experiencing stretch and communicate information about muscle length.
Within the spinal cord, a single sensory 1a afferent axon synapses on every alpha motor neuron within the motor pool that innervates the muscle that contains the muscle spindle. This allows for a fast and powerful contraction of the muscle in response to a change in muscle stretch.
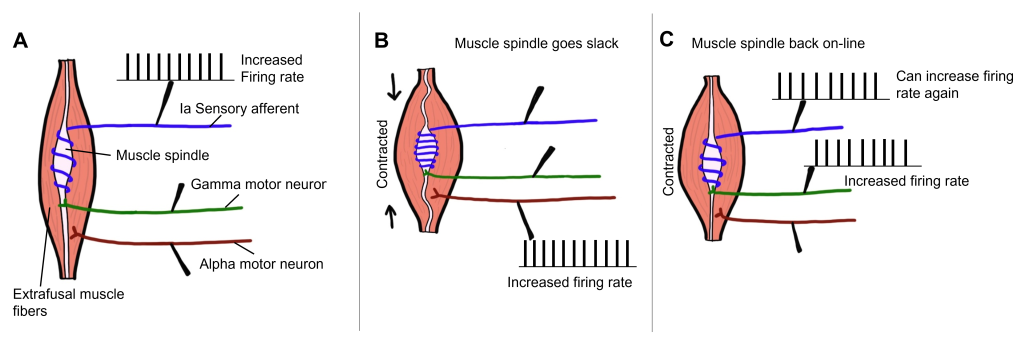
Gamma Motor Neuron Function
When the muscle experiences a stretch and the extrafusal fibers are stretched, the muscle spindle and the intrafusal fibers are also stretched (due to being within the muscle and surrounded by the extrafusal fibers). When the muscle spindle stretches, the 1a sensory axon will start to fire action potentials. The sensory axon synapses with an alpha motor neuron that will then cause the extrafusal muscle fibers to contract. As the extrafusal fibers contract and the muscle shortens, the muscle spindle goes slack, and the 1a axon will no longer fire action potentials as it is no longer being stretched. The gamma motor neuron is then activated that innervates the intrafusal muscle fibers, causing the intrafusal fibers to contract, allowing the muscle spindle to sense stretch again. Therefore, the gamma motor neuron is critical for allowing the muscle spindle to continue providing information about muscle stretch even when the muscle has experienced contraction.
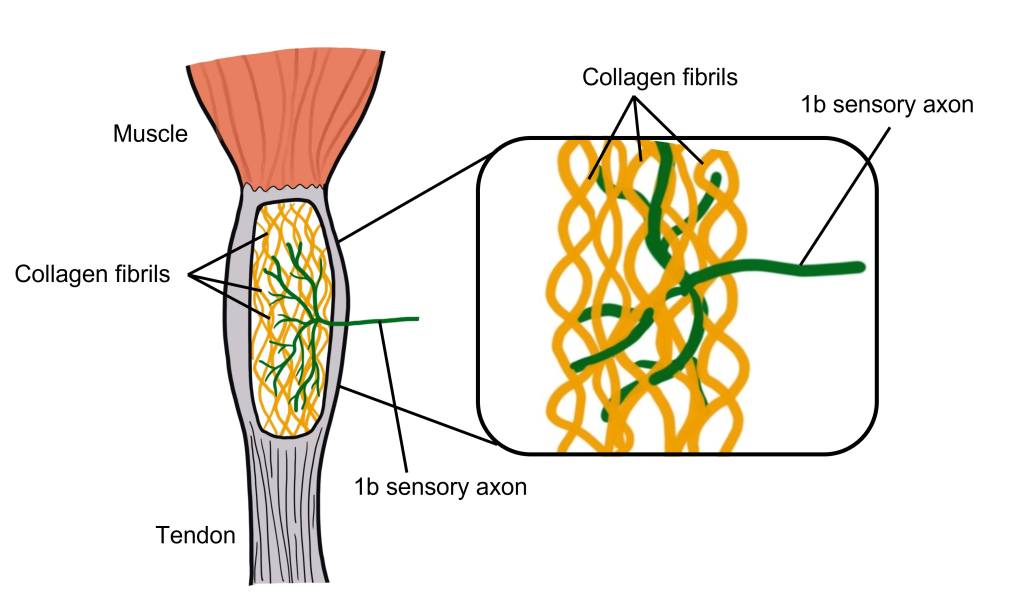
Golgi Tendon Organ
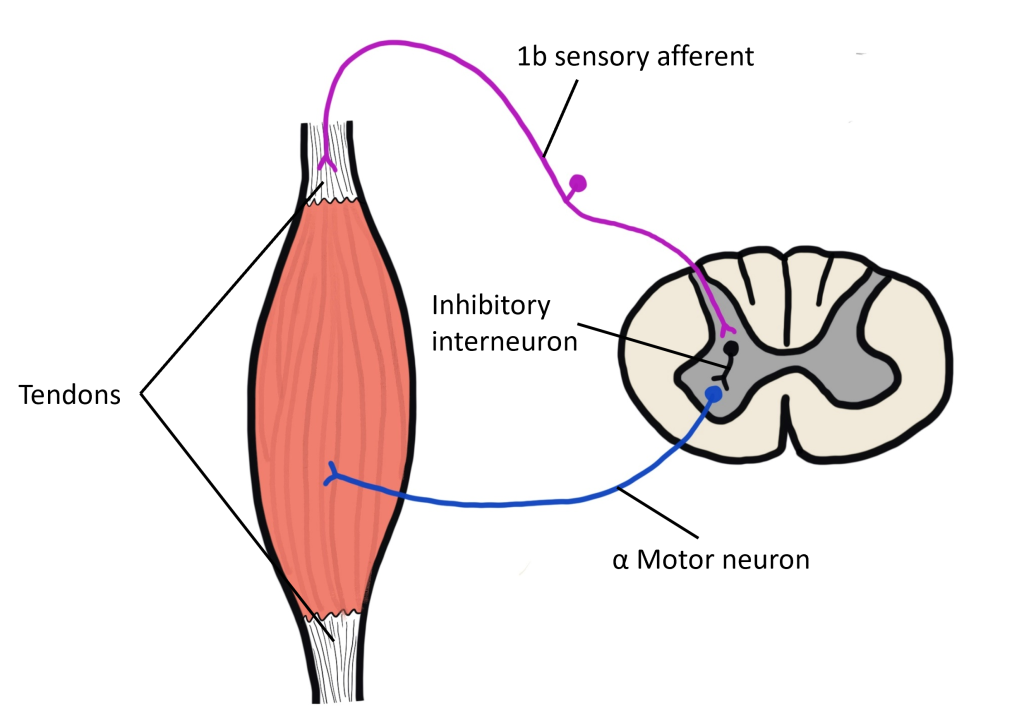
The Golgi tendon organ is a proprioceptor that measures muscle tension, or the force of contraction. They also contribute to our detection of weight, as we lift something heavy for example. Golgi tendon organs are located in the tendon that connects the muscle to bone. The tendon is made up of collagen fibrils and the Group 1b sensory axons are intertwined within the collagen fibrils. When the muscle experiences an increase in tension, the collagen fibrils surrounding the 1b sensory axon physically squeeze the 1b axon, opening mechanically-gated ion channels within the 1b sensory axon.
The purpose of the Golgi tendon organ is to allow for an optimal range of tension for the muscle and to protect the muscle from injury due to being overloaded. This is accomplished through a negative feedback loop controlled by the Golgi tendon organ. When the muscle experiences an increase in muscle tension, the 1b sensory axon starts to fire action potentials. The sensory neuron synapses onto an inhibitory interneuron within the spinal cord, which when active will release GABA onto the alpha motor neuron that innervates the same muscle that experienced the increase in muscle tension to begin with. When GABA binds to the alpha motor neuron, it will decrease firing of the alpha motor neuron, leading to a decrease in contraction of the muscle. This is an example of negative feedback as the increased muscle tension ultimately leads to physiological changes that decrease muscle tension.
Key Takeaways
- Motor neuron cell bodies are located in the ventral horn of the spinal cord.
- Motor neuron axons are located in the peripheral nervous system and travel to muscles via spinal nerves.
- Acetylcholine is released at the neuromuscular junction and acts upon ionotropic nicotinic acetylcholine receptors.
- The spinal cord is topographically organized.
- Muscle twitches can summate to increase muscle tension.
- A motor unit is an alpha motor neuron and all of the motor fibers that it innervates. Motor units differ in size, recruitment, and power.
- Muscle spindles and Golgi tendon organs are proprioceptors that communicate information about the location and position of the body.
Test Yourself!
Additional Review
- What is the difference between a motor unit and a motor pool?
Attributions
This chapter is adapted from “Spinal Motor Control and Proprioception” in Introduction to Neuroscience by Valerie Hedges which is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Media Attributions
- MotorControlRegions © Casey Henley adapted by Valerie Hedges is licensed under a CC BY-NC-SA (Attribution NonCommercial ShareAlike) license
- Alpha Motor Neuron © Casey Henley adapted by Valerie Hedges is licensed under a CC BY-NC-SA (Attribution NonCommercial ShareAlike) license
- Spinal Cord Map © Casey Henley adapted by Valerie Hedges is licensed under a CC BY-NC-SA (Attribution NonCommercial ShareAlike) license
- Untitled_Artwork 1 © Casey Henley adapted by Valerie Hedges is licensed under a CC BY-NC-SA (Attribution NonCommercial ShareAlike) license
- NMJ Ion Flow © Casey Henley adapted by Valerie Hedges is licensed under a CC BY-NC-SA (Attribution NonCommercial ShareAlike) license
- NeuromuscularJunction © Casey Henley adapted by Valerie Hedges is licensed under a CC BY-NC-SA (Attribution NonCommercial ShareAlike) license
- Myasthenia Gravis © Posey and Spiller adapted by Valerie Hedges is licensed under a Public Domain license
- Motor Unit And Pool © Casey Henley adapted by Valerie Hedges is licensed under a CC BY-NC-SA (Attribution NonCommercial ShareAlike) license
- Types of motor units © Valerie Hedges is licensed under a CC BY-NC-SA (Attribution NonCommercial ShareAlike) license
- Muscle_Twitch_Myogram © OpenStax adapted by Valerie Hedges is licensed under a CC BY (Attribution) license
- Twitch_vs_unfused_tetanus_vs_fused_tetanus © Daniel Walsh and Alan Sved adapted by Valerie Hedges is licensed under a CC BY-SA (Attribution ShareAlike) license
- Motor unit recruitment © Daniel Walsh and Alan Sved is licensed under a CC BY-SA (Attribution ShareAlike) license
- Motor neuron inputs © Valerie Hedges is licensed under a CC BY-NC-SA (Attribution NonCommercial ShareAlike) license
- Muscle Spindle © Casey Henley adapted by Valerie Hedges is licensed under a CC BY-NC-SA (Attribution NonCommercial ShareAlike) license
- Gamma motor neuron function © Valerie Hedges is licensed under a CC BY-NC-SA (Attribution NonCommercial ShareAlike) license
- Golgi tendon organ © Valerie Hedges is licensed under a CC BY-NC-SA (Attribution NonCommercial ShareAlike) license
- golgi tendon organ signaling © Valerie Hedges is licensed under a CC BY-NC-SA (Attribution NonCommercial ShareAlike) license
traveling from the CNS to the body
Toward the edge
Toward the middle
The synapse between a motor neuron and a muscle fiber
a motor neuron and all of the muscle fibers that is innervates
The group of motor neurons that innervate all the fibers of one muscle
Body sense that allows for understanding of location and position of body parts
sensory receptors that provide information about proprioception
proprioceptors that communicate muscle length (muscle stretch)
muscle fibers that are located inside of the muscle spindle capsule
muscle fibers that are outside of the muscle spindle capsule. Extrafusal fibers make up the bulk of the muscle.
Proprioceptor that communicates information about muscle length
Proprioceptor that measures muscle tension